STORYBOX : David has migraine [1] attacks a few days per month, with light sensitivity and nausea. When he was a kid, he was car sick. Last year, he woke up one morning with severe vertigo and could not walk. He went to the ED and received a diagnosis of labyrintitis. The episode lasted a few days then resolved. Since then, his migraines have changed. They sometimes start with vertigo, and during the headache phase David is very dizzy. He cannot drive. On occasions, he will have a few days with dizziness [2] and vertigo, but no headaches. What is going on? He saw an ENT doctor, did vestibular testing, and was sent to the neurologist.
What does «vestibular» mean?
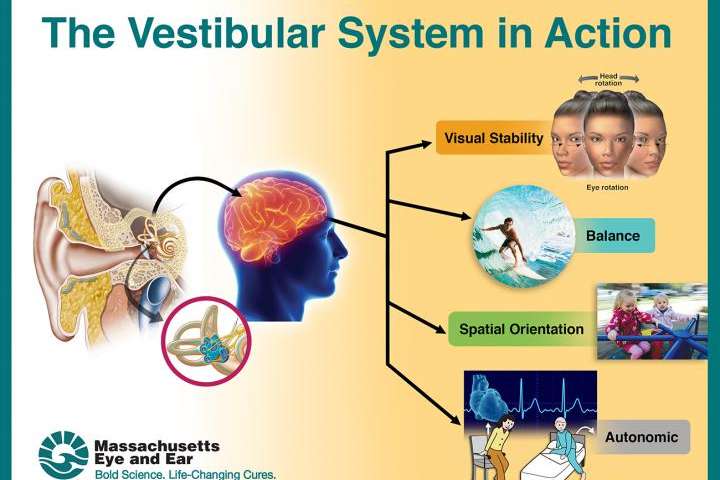
Vestibular refers to the organs of balance in the ear and all the system gathering the information on our head and body’s position. The vestibular system allows us to be stable, walk, and focus our eyes on targets. The vestibular system is very close to the auditory system.
If there is a problem with the vestibular system, what are the symptoms?
Vertigo is a sensation of motion, often spinning. Dizziness is difficult to define, but often implies some feeling of instability. Oscillopsia means that the eyes seem to shake. The ability to walk straight can be impaired. Nausea and vomiting often are present. Since the auditory organs are close and use the same nerve (8th) for transmission of information to the brain, abnormal hearing can accompany vestibular symptoms.
What is vestibular migraine?
Vestibular migraine (VM) is a combination of migraine and vestibular symptoms (dizziness, vertigo). According to our Classification, 50% of vestibular attacks have to be accompanied by migraine symptoms (sensory intolerance, headache). The description of vestibular migraine is still ongoing, as many combinations of symptoms may occur.
People who suffer from VM frequently report that the dizziness can be triggered by seeing things in motion, especially in crowded areas (shopping centers, busy crowds). We call this phenomenon «visually induced vertigo/dizziness».
Vestibular migraine seems more common in people who have auras and people with chronic migraine [3].
How does vestibular migraine begin?
Two things can happen. Either the person already has a clear history of migraine and then develops vestibular symptoms, or both the vestibular symptoms and migraines start at the same time.
If the vestibular symptoms were caused by trauma to the head or neck, and the headache are also the consequence of trauma, then the diagnosis should be post-traumatic headache [4].
Could headache and vertigo be caused by other conditions than VM?
Of course! It is very important to get an ENT evaluation to exclude conditions like Benign Paroxysmal Positional Vertigo, Meniere’s Disease and any abnormality of the vestibular system. It is possible for someone with migraine to have a completely separate vestibular problem that needs specific treatment. (See this post [5])
Is there a reliable test to diagnose Vestibular Migraine?
Sadly, no. Vestibular Testing should be done, but can be normal in 40% of people. Sometimes, abnormalities can be found on testing, but are not exclusive to VM. There is no imaging test for VM, but an MRI will often be done to exclude other things.
Is Vestibular Migraine a real medical issue?
Yes. Research suggests that 1% of the population suffers from this syndrome. But research is ongoing, and many elements of this puzzle are controversial, mostly because we lack a reliable diagnostic test. The symptoms of VM can be quite disabling and impair the ability to read, drive, walk and even stand.
What is the cause of Vestibular Migraine?
That’s a difficult question, as the vestibular networks are very complex, and the migraine networks are as well. Many scenarios can be proposed. The problem could be that the hyperexcitable migraine brain becomes hypersensitive to motion. Inflammation [6] (including CGRP release) could occur in the vestibular system. Vestibular symptoms could be part of an aura [7] (a wave of electricity on the cortex). Research is ongoing.
What treatments can be used for Vestibular Migraine attacks?
Treatments used for typical migraine (NSAIDs, triptans [8]) are often used. Since VM can come with severe nausea, anti-emetics are often part of the combination. Dizziness can be helped by anti-histamine drugs (a bit like sea/car sickness) and they can be used, but may also cause somnolence.
What medications can decrease the frequency of VM attacks?
Once again, migraine preventives are usually tried, with some success. Studies suggest that venlafaxine (Effexor), topiramate [9] (Topamax) and calcium channel blockers (like flunarizine/Sibelium) may be more effective for VM. There are anecdotes about Botox improving vestibular symptoms, but more research is definitely needed. We have no data on CGRP MABs for now.
Should I try vestibular physiotherapy?
Vestibular physiotherapy [10] uses exercises to reinforce vestibular reflexes when the ear organs have been injured. The problem with the migraine brain is that it does not manage the reflexes normally. Vestibular physiotherapy may be challenging for a migraine patient [11], and take more effort to be effective.
This being said, if there is a diagnosis of BPPV, physio can be extremely helpful. Also, dizziness, vertigo and migraine are strongly associated with anxiety, and anxiety increases these symptoms in a very vicious cycle. Therefore, relaxation techniques, meditation [12] and anxiety management can really improve the quality of life of people with VM.
REFERENCES
Lempert T, von Brevern M. Vestibular Migraine. Neurol Clin. 2019;37(4):695-706.
Post#106
