What is idiopathic intracranial hypertension?
The pressure inside the head should be stable. Imagine a car tire: if the pressure’s too low, it gets flat (in the head that causes the intracranial hypotension syndromes), and if it’s to high it can damage the tire.
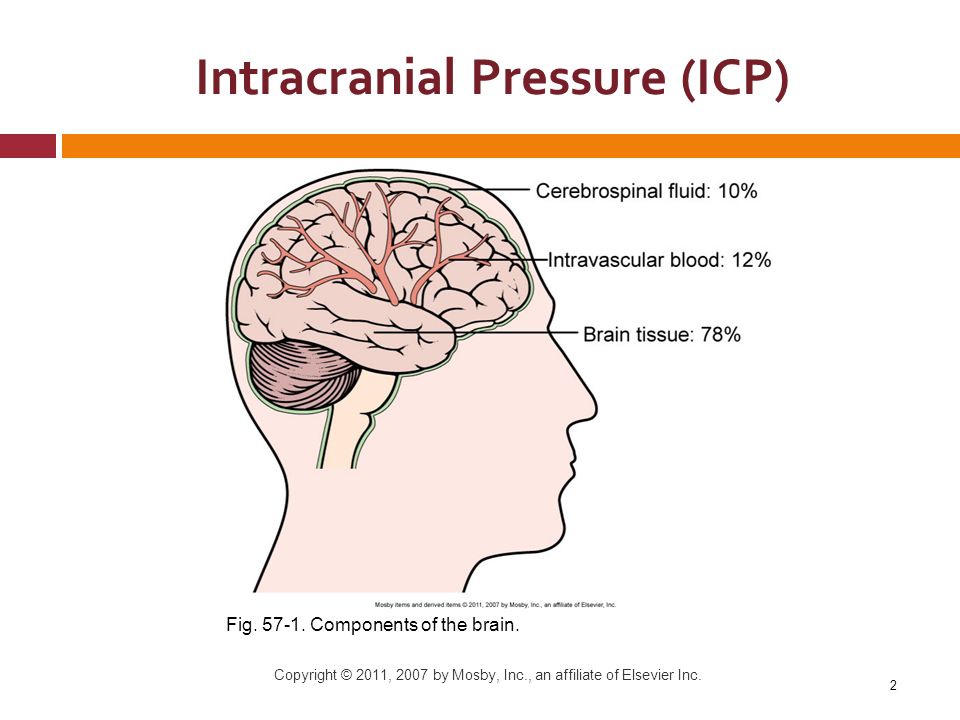
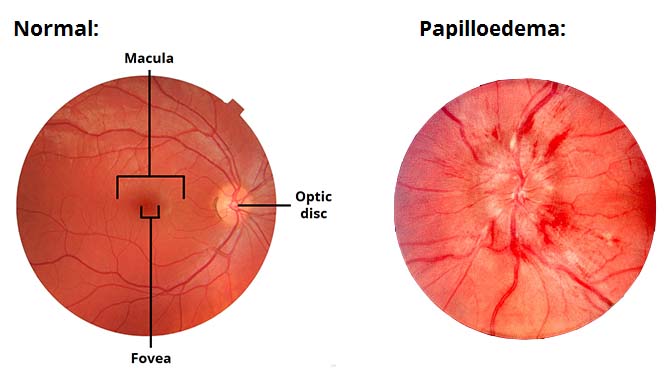
Idiopathic intracranial hypertension is a disease where the mechanisms that keep the pressure inside the head within normal limits are disrupted. The pressure increases, leading to headaches and swelling of the optic nerves that can threaten vision.
What are the typical symptoms of IIH?
- Headache is the most common symptoms (90% of patients). The headache is usually diffuse, moderate, and may be throbbing. It may be worse when lying down (as the pressure increases in this position).
- Nausea and vomiting can occur.
- The swelling of the optic nerve leads to visual problems: seeing black when bending over, seeing stars, losing peripheral vision (not always evident as we focus on our central vision).
- The pressure also impacts the nerves that make the eyes move, and that can cause double vision (diplopia).
- If the pressure impacts the auditory nerves, tinnitus might occur, sometimes pulsatile and worse when lying down or bending over.
What is the cause of IIH?
We do not know yet the exact cause, but we have hypotheses. It seems that the brain with IIH does accumulate too much liquid diffusely in the brain (a bit like edema) and that may increase the pressure.
How can we confirm the diagnosis of IIH?
If your symptoms are suggestive, then you should be evaluated by a neuro-ophtalmologist to check your optic nerves and visual fields. If there is swelling of the nerves (called papilledema) and loss of vision, different treatments can be offered.
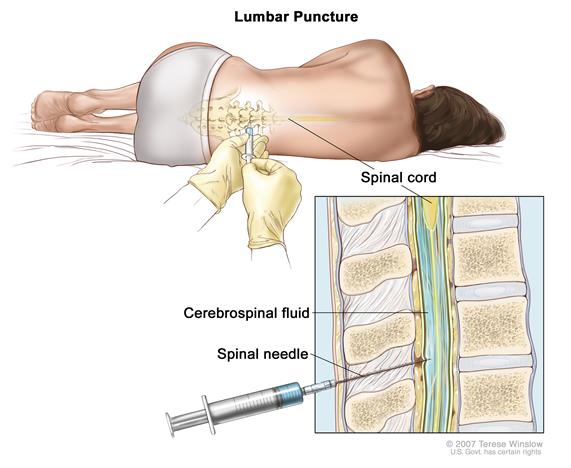
All patients with IIH should have an MRI of the brain and a lumbar puncture to measure the pressure at least once. If the optic nerves are normal and the pressure is not elevated, then other causes of chronic headaches must be considered (including chronic migraine [1]).
Are there other causes of high intracranial pressure?
Many of them. Any mass (tumor, abcess) inside the head can raise the pressure. A blockage of veins (venous thrombosis) must be excluded with proper imaging (CT or MRI). Disorders of coagulation seem to be linked as well, and people with lupus may develop high pressure as well. Medications like Accutane and certain antibiotics may cause this syndrome.
I had migraine before developing IIH. Is that common?
Yes. 40% of people with IIH have a history of migraine [2], and that is more than what is seen in the general population (15%). IIH is seen more commonly in women in their reproductive period, who are more prone to have migraine, but still there seems to be a link between both. When there is a history of migraine, the physician might propose topiramate [3] and Botox as options to control the headaches.
I was told that I must lose weight. Why would this change my pressure?
Obesity is very strongly linked with IIH, therefore, weight loss is key to treat this problem. Physicians with experience in this field know that weight loss (even 10% of body weight) can make a huge difference in symptoms, but also know that weight loss is not easy. All possible efforts must be made to lose weight as this could save vision. See more on weight loss here [4].
This being said, only a small fraction of obese people have IIH, that means that there are other factors at play to cause this condition. Many women who have chronic headaches and are obese or overweight have chronic migraine, not IIH.

Are there medications available to treat IIH?
- Acetazolamide, a diuretic (a medicine that increase urine volume), is the usual drug to start with. There is proof that ACTZ will improve vision, but may not be as effective to treat headaches. Side effects [5] include nausea, tingling in the extremities and fatigue.
- Metazolamide is a cousin drug of acetazolamide and might be better tolerated.
- Topiramate, used for epilepsy and migraine, is also used. It has more side effects like memory , word finding and focus difficulties, but it may be better for the headaches. It may also promote weight loss.
- Any drug causing weight gain (like amitriptyline [6]/Elavil) should be avoided. Some physicians recommend to stop oral contraceptives but there is no evidence that this should be done.
Can we just drain the fluid out with a shunt?
This approach, shunting, has been tried. It is an invasive surgery, during which a tube is placed to link the fluid in the brain ventricles to the belly (ventriculo-peritoneal shunt) or to link the CSF space in the spine with the belly space (lumbo-peritoneal shunt). Both techniques have a high rate of complications and should not be used unless vision is severely threatened, under the supervision of an expert team.
Will I lose my vision because of IIH? What can I do to prevent this?
Visual loss does occur with IIH, it is a serious risk. A regular eye exam done by an ophthalmologist or optometrist is part of the follow-up. If symptoms recur or increase, then a vision test should be urgently repeated to look at the optic disk and visual fields.
Other resources on Idiopathic Intracranial Hypertension
REFERENCES
- Ahmad SR, Moss HE. Update on the Diagnosis and Treatment of Idiopathic Intracranial Hypertension. Semin Neurol. 2019;39(6):682-91.
- Friedman DI. Contemporary management of the pseudotumor cerebri syndrome. Expert Rev Neurother. 2019;19(9):881-93.
- Ganesh A. Idiopathic intracranial hypertension: need to rule out cerebral venous sinus thrombosis. Cmaj. 2019;191(40):E1109.
- Thurtell MJ. Idiopathic Intracranial Hypertension. Continuum (Minneap Minn). 2019;25(5):1289-309.
Post#403
