Understanding the intricate link between neck pain, migraine, and cervicogenic headaches is crucial for effective treatment and management. In this post, we delve into the complex relationships among these conditions through the real-life stories of Mandy, Paul, and Tamara. Each narrative illustrates how posture, trauma, and chronic conditions can intertwine to exacerbate neck pain and migraine. This comprehensive guide explores the anatomy and neural connections involved, diagnostic challenges, and potential treatment options for those suffering from these debilitating headaches.
Mandy

Mandy, 27, has had migraine since she’s 15. She has more migraine during her period. Her usual frequency is 10 days per month. She’s tall, lean, and has hyperextensible joints. She used to practice yoga and light weights, but now she’s working full time as a market analyst and she’s sitting most of the day. At night, she’s exhausted and watches TV. Since one year, she has developed neck pain, and more recently jaw pain. Her posture is slouching. Her migraine developed during the day. She tried amitriptyline but was too somnolent with it and stopped.
Neck pain can be caused by a bad posture and trigger migraine. Jaw pain can accompany neck pain.
Paul

Paul, 56, had very occasional migraine with aura. In fact, they are now happening a few times per year. Last year, Paul had a car accident with a whiplash. Since this event, he has chronic neck tensions and his migraine have reappeared, but now are starting with a deep pain on the right side of his neck. Sometimes he also feels a burning and some ice picks. An occipital nerve block provided him relief for a few weeks.
Neck pain can be caused by a trauma and trigger migraine. Occipital neuralgia can accompany other types of neck pain.
Tamara

Tamara, 42, has chronic migraine. She rarely has a day without some headache. She never had head trauma. She exercises gently a few times per week with a program designed by a physio. Despite all this, when a migraine starts, she feels a lot of tension in her neck and down the shoulders. She tried a few preventives, with no success. Interestingly, after three treatments of Botox, her migraine is 70% better and the neck pain is gone.
Neck pain can be caused by migraine in a person with a normal neck and posture.
Anatomy Fact
In humans, the head and the neck pain networks are linked and can cross-talk (see image below).
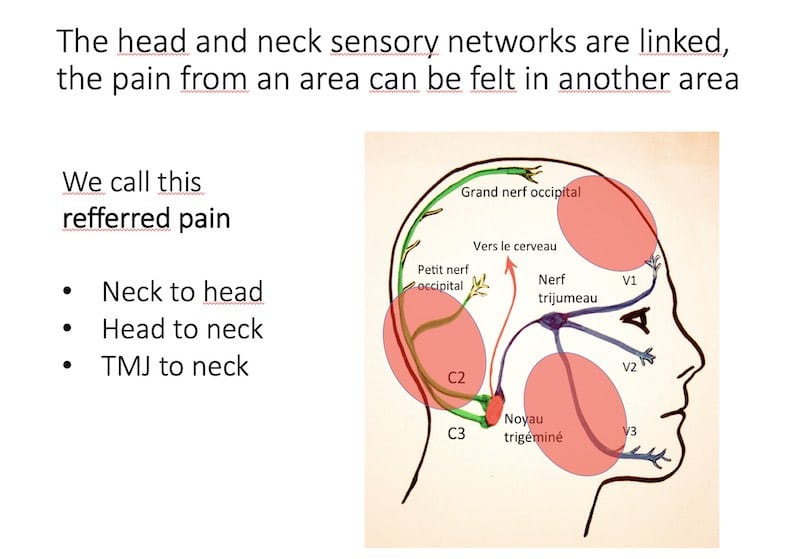
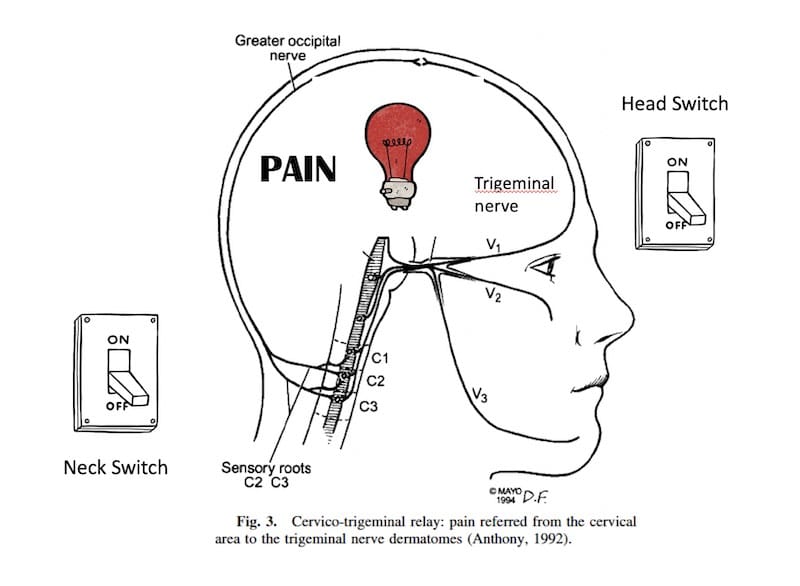
Head and neck pain networks are linked, explaining their frequent association. The trigeminal nerve carries sensations from the face and head, while the cervical nerves (C2-C4) handle neck and shoulder sensations. Both networks connect at the trigeminal nucleus, like different switches activating the same light bulb (see image below).
What is a cervicogenic headache?
In theory, cervicogenic headache is a headache that is caused by a problem in the neck. A cervical nerve block should provide significant relief as it treats “the cause” of the problem. This definition does not address two very common situations: a person with migraine who has neck pain and a person who has post-traumatic headache with neck pain.
Migraine ping pong theory: Neck version
A neck problem can cause migraine, and a migraine can cause neck pain. Moreover, a bad migraine might trigger a contraction in the shoulder muscles, creating a vicious circle of pain. Severe migraine might also decrease the ability to exercise and contribute to deconditioning. In this situation, the neck is part of the problem, but not the “only cause.” For more information, see our post on the ping pong theory.
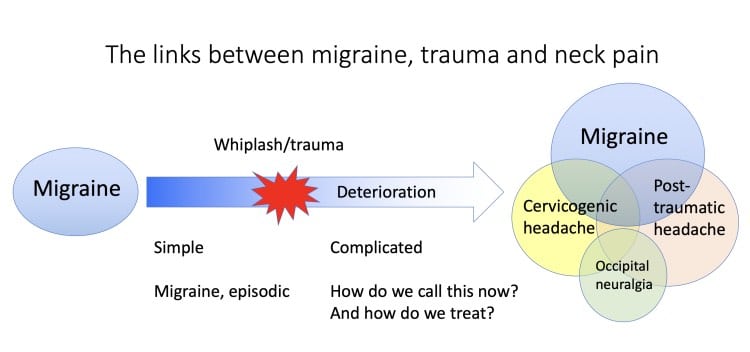
The complicated case of post-traumatic headache
Traumas may cause persistent neck pain, and in fact, most cervicogenic headache research is done on people who have post-traumatic headache. This confusion in the classification is not helpful to patients and hopefully will be adapted in the future. Considering the fact that migraine is a risk factor for persistent symptoms after a trauma, you can get into a situation with multiple factors, and this situation is common in real life.
Occipital neuralgia: What is it?
Pain from a specific nerve problem, often electrical, with sensory deficits. Misdiagnosed in many migraine patients due to similar symptoms like allodynia.
How does the physician diagnose cervicogenic headache?
There is no unique answer to this question, as there is still a lot of controversy about this. In theory, Cervicogenic headache excludes people with migraine and trauma. There are no reliable tests to diagnose cervicogenic headache.
One technique used as a diagnostic test is to do a C2-C3 blockade and see if the headache gets better, proving the origin of the problem. But this technique is not perfect. It can lead to a placebo response or to a failure in a refractory situation still caused by a neck issue.
What can be done to treat cervicogenic headache?
A comprehensive approach involving physiotherapy, medications, and pain management techniques is common. Chiropractors and osteopaths may be consulted, but their methods are controversial in traditional medicine. Long-term management is often required.
References
- Bogduk N, Govind J. Cervicogenic headache: An assessment of the evidence on clinical diagnosis, invasive tests, and treatment. Lancet Neurol. 2009;8(10):959-68.
Post #401



