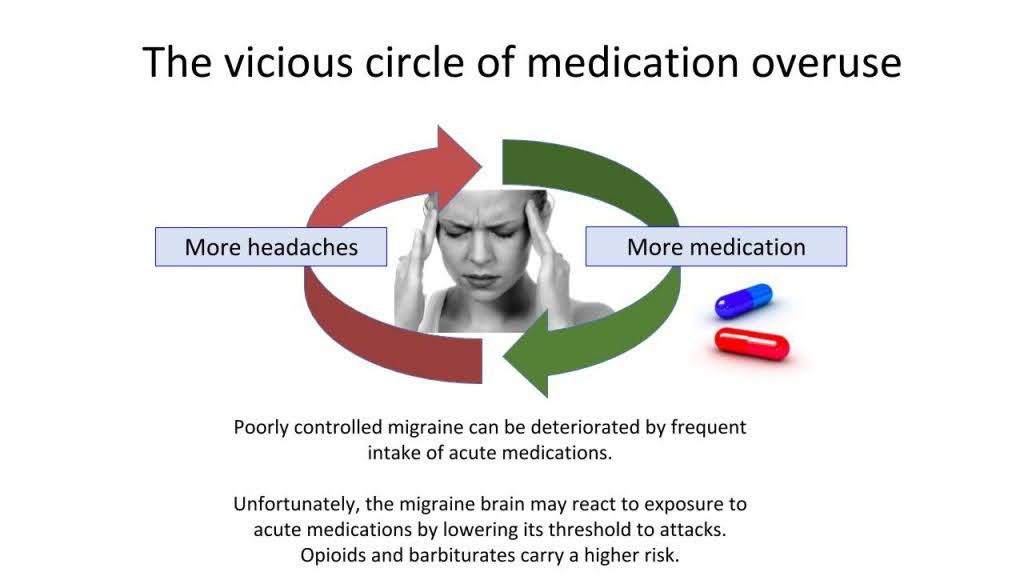
In this post, we delve into the complexities of Medication Overuse Headache. Often triggered by frequent medication use, this condition significantly impacts those living with chronic migraine. Explore implicated medications and discover effective strategies for withdrawal and management. Gain valuable insights into the challenges of treatment and the critical role of medication management to prevent recurrence.
What is medication overuse headache?
A headache caused by the regular use of certain medications. This headache is present on 15 or more days per month for 3 months or longer, in a person who uses medications on 10-15+ days per month.
How do we know that medications cause headaches?
Scientific studies show that stopping medication overuse for at least 3 months improves headaches in 60-70% of people.
Am I alone in this situation?
No. About 1% of the global population is affected. Nearly 50% of people with chronic migraine experience medication overuse headaches.
What medications can cause it, and how much is too much?
Most migraine medications can cause overuse headaches. Treating more than 2 days per week can be risky.
Medication | Monthly days of use linked with chronification |
Opioids (Fiorinal, codeine) | 10+ |
Triptans (Zomig, Imitrex) | 10+ |
NSAIDs/simple painkillers (Tylenol, Advil) | 15+ (if only one type is used) |
Any combination of acute treatments | 10+ |
Who can develop medication overuse headache?
People with migraine or tension-type headaches are more susceptible due to their brain’s response to medications.
Am I dependent or addicted?
Not necessarily. The brain adapts to regular pain medication, making pain networks more active, leading to more headaches. This is usually not addiction but a response to frequent medication use. However, opioids and barbiturates can be addictive.
What can I do?
Stop the offending medications with your doctor’s guidance. Daily preventive medications might be necessary. Overuse may block their effects.
How will I treat my headache during withdrawal?
Alternative treatments may be used. Withdrawal can be tough and needs careful planning.
What can I expect while stopping?
Headaches may worsen for 3-4 weeks as the brain resets. Improvement is seen in 4-8 weeks. Headaches may not disappear but will be less frequent. Keep a diary to track progress.
How will I treat my headaches in the future?
Preventive medications might be needed for at least 3 months. Rescue medications can be used again but less frequently.
Can this situation come back?
Yes. Your brain will remain vulnerable. Adhere to safe medication limits to avoid recurrence.
What if I need Tylenol or opioids for another reason?
Short-term use is fine. For use longer than 3 months, consult your doctor. Using opioids for chronic headaches is rarely effective and should be managed by a specialist.
Medication overuse headache is highly treatable. Your wellness is within your control!
To read more, visit our other posts on Medication Overuse Headache: What Is It and Why Is It Happening? and Medication Overuse Headache: Tips to Organize a Successful Withdrawal.
Case Example:
“For years, I regularly took Tylenol codeine and Zomig. I did not know it could cause medication overuse headache. After a few years, these drugs did not work very well for me, so I had to take more and more. Sometimes I ended up in the emergency room. Eventually, I was prescribed Dilaudid. No preventive medications worked. Since I stopped overusing medications, I still have migraine, but I do not have this constant head pain anymore. Now my preventive medications are working better and I respond better to triptans when I get a migraine.”
References
- Chiang CC, Schwedt TJ, Wang SJ, Dodick DW. Treatment of medication-overuse headache: A systematic review. Cephalalgia. 2016;36(4):371-86.
- Diener HC, Holle D, Solbach K, Gaul C. Medication-overuse headache: risk factors, pathophysiology, and management. Nat Rev Neurol. 2016;12(10):575-83.
- Tepper SJ, Tepper DE. Breaking the cycle of medication overuse headache. Cleve Clin J Med. 2010;77(4):236-42.
Post #105



