Sleep apnea and migraine are two prevalent but often interconnected conditions that can significantly impact an individual’s quality of life. Sleep apnea, characterized by disruptions in breathing during sleep, is known to cause morning headaches and may worsen chronic migraine symptoms. This comprehensive overview explores the link between sleep apnea and migraine, detailing the types of headaches caused by sleep apnea, potential risk factors, diagnostic tests, and treatment options. If you experience morning headaches, snoring, or worsening migraine, understanding this connection and seeking appropriate medical evaluation can be crucial.
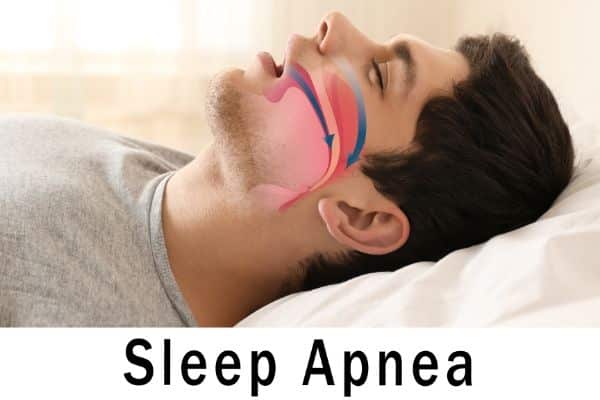
What is sleep apnea?
Sleep apnea is a condition characterized by disruptions in breathing during sleep. This can occur due to a blocked airway or a pause in the brain’s signal to breathe. As a result, the individual may experience low oxygen levels, leading to sudden gasping for air and resumed breathing.
What types of headaches can be caused by sleep apnea?
Typically, headaches caused by sleep apnea are called “morning headaches.” They are present on awakening and tend to improve over a few hours. They can look like tension headaches or migraine. In one study, 20% of people diagnosed with sleep apnea had morning headaches.
Is there a link between migraine and sleep apnea?
People with chronic migraine are more at risk for sleep apnea. Sleep disorders increase the risk of chronic headaches. There are many histories of migraine that deteriorated in the setting of sleep apnea improving with CPAP (continuous positive airway pressure) treatment. We do not know yet exactly how many people with chronic migraine have sleep apnea.
Why would apnea cause headaches?
Obviously, we breathe for a reason. When we stop breathing, the oxygen in our blood decreases and the carbonic gas increases. This triggers different reactions in the body, like hypertension. These nighttime metabolic changes are believed to contribute to the onset of morning headaches. The fragmented sleep caused by apneas can result in daytime drowsiness, fatigue, and consequently impact migraine conditions.
What are symptoms that could suggest that I have sleep apnea?
-
- Habitual snoring
- Witnessed apnea
- Waking gasping or choking
- Headache upon waking
- Hypersomnia (or insomnia)
- Night sweats
What are risk factors for sleep apnea?
While obesity, advanced age, and male gender are common risk factors for sleep apnea, other considerations include:
-
- Wide neck (male > 17˝ and female > 16˝)
- Born female gender post-menopause
- Older age
- Family history (especially multiple family members)
- Small chin or jaw (micrognathia)
- Mouth/throat anatomy: Large tongue, tonsils
- Neuromuscular disorders
- Substances (e.g., tobacco, alcohol, sedatives, opiates, muscle relaxants)
What tests are available for sleep apnea?
- Polysomnography: Overnight monitoring attended by technologist in a sleep lab
- Portable cardiorespiratory monitoring home sleep apnea test (HSAT) at home
The key result of testing is usually the Apnea Hypopnea Index (AHI). 5-15 is mild, 15-30 is moderate, and greater than (>) 30 is severe.
What are treatment options?
- Conservative measures: Positional therapy to avoid supine sleep, smoking cessation, non-surgical weight loss
- Avoidance of alcohol, muscle relaxants, anxiolytics, opiates, sedatives, and hypnotics)
- Positive airway pressure (continuous or CPAP, bilevel PAP)
- Oral appliances (mandibular advancement devices, tongue retaining devices)
- Surgery of the upper airway
- Hypoglossal nerve stimulation
- Bariatric surgery for weight loss
- Nocturnal oxygen (case-by-case basis)

The CPAP mask is not always easy to tolerate. The pressure can even trigger migraine attacks. Given the challenges some individuals face with CPAP masks, exploring alternative treatments with a sleep medicine specialist is advisable.
The coverage of testing and treatments varies a lot. Considering the health consequences of untreated sleep apnea, it would be an advantage to our society to see this covered by public insurance.
In summary, for those experiencing worsened migraine, snoring, or morning headaches, discussing sleep apnea testing with a healthcare provider is recommended.
References
- Buse DC, Rains JC, Pavlovic JM, Fanning KM, Reed ML, Manack Adams A, et al. Sleep Disorders Among People With Migraine: Results From the Chronic Migraine Epidemiology and Outcomes (CaMEO) Study. Headache. 2019;59(1):32-45.
- Ferini-Strambi L, Galbiati A, Combi R. Sleep disorder-related headaches. Neurol Sci. 2019;40(Suppl 1):107-13.
- Rains JC. Sleep and Migraine: Assessment and Treatment of Comorbid Sleep Disorders. Headache. 2018;58(7):1074-91.
Post #203



