Vestibular migraine is a complex and often misunderstood condition, blending migraine symptoms with vertigo and dizziness. In this detailed account, we’ll explore David’s story to illustrate the impact of vestibular migraine on daily life. We’ll define key terms, explain the vestibular system, and discuss the symptoms and causes of vestibular migraine. Additionally, we’ll review diagnostic challenges, treatment options, and the importance of multidisciplinary care. This comprehensive guide aims to provide valuable insights for those affected by vestibular migraine and their healthcare providers.
David’s Story
David experiences migraine attacks a few days per month, often accompanied by light sensitivity and nausea. As a child, he suffered from car sickness. Last year, he woke up one morning with severe vertigo and couldn’t walk. After visiting the emergency department, he was diagnosed with labyrinthitis. The episode lasted a few days and then resolved. Since then, his migraine has changed. The attacks sometimes start with vertigo, and during the headache phase, David feels very dizzy and cannot drive. Occasionally, he experiences dizziness and vertigo for a few days without head pain. What is going on? He saw an ENT (ear, nose, and throat) doctor, underwent vestibular testing, and was referred to a neurologist.
What does “vestibular” mean?
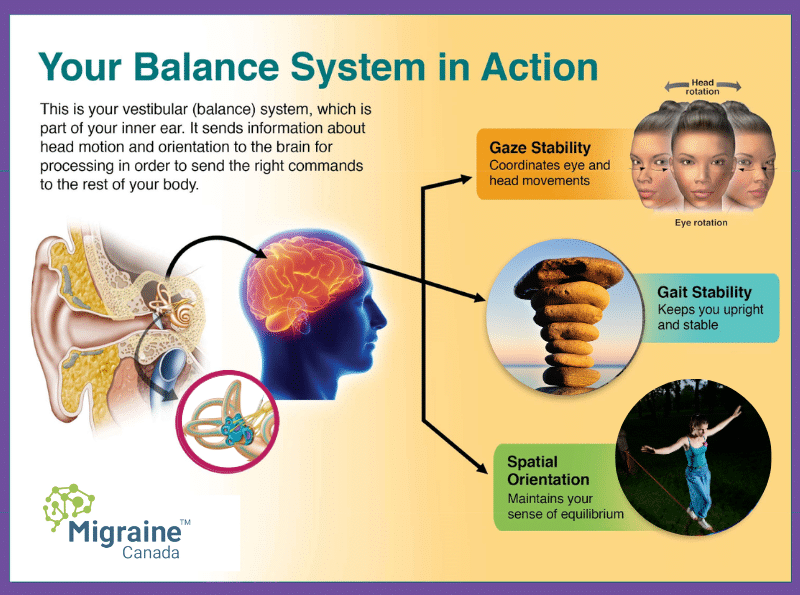
Vestibular refers to the organs of balance in the ear and the system that gathers information about our head and body’s position. The vestibular system allows us to maintain stability, walk, and focus our eyes on targets. It is closely related to the auditory system.
If there is a problem with the vestibular system, what are the symptoms?
Vertigo is a sensation of motion, often spinning. Dizziness is difficult to define but often implies a feeling of instability. Oscillopsia means that the eyes seem to shake. The ability to walk straight can be impaired. Nausea and vomiting are often present. Since the auditory organs are close and use the same nerve (the 8th cranial nerve) for transmitting information to the brain, abnormal hearing can accompany vestibular symptoms.
What is vestibular migraine?
Vestibular migraine (VM) is a combination of migraine and vestibular symptoms (i.e., dizziness, vertigo). According to our classification, 50% of vestibular attacks must be accompanied by migraine symptoms (e.g., sensory intolerance, headache). The description of vestibular migraine is still ongoing, as many combinations of symptoms may occur.
People who experience VM frequently report that the dizziness can be triggered by seeing things in motion, especially in crowded areas like shopping centers and busy crowds. This phenomenon is called “visually induced vertigo/dizziness.” Vestibular migraine seems more common in people who have aura and chronic migraine.
How does vestibular migraine begin?
Two scenarios can occur. Either the person already has a history of migraine and then develops vestibular symptoms, or both the vestibular symptoms and migraine attacks start simultaneously.
If the vestibular symptoms were caused by trauma to the head or neck, and the headache is also the consequence of trauma, then the diagnosis should be post-traumatic headache.
Could headache and vertigo be caused by other conditions than vestibular migraine?
Of course! It is crucial to get an ENT evaluation to exclude conditions like Benign Paroxysmal Positional Vertigo (BPPV), Meniere’s Disease, and any abnormalities of the vestibular system. It is possible for someone with migraine to have a completely separate vestibular problem that needs specific treatment. Migraine could be the cause or the consequence, as discussed in this post on ping pong theory.
Is there a reliable test to diagnose vestibular migraine?
Unfortunately, no. Vestibular testing should be done, but results often come back normal in 40% of people. Sometimes, abnormalities can be found on testing but are not exclusive to VM. There is no imaging test for VM, but an MRI will often be done to exclude other conditions.
Is vestibular migraine a real medical issue?
Yes. Research suggests that 1% of the population experiences this condition. However, research is ongoing, and many aspects are controversial, mostly due to the lack of a reliable diagnostic test. The symptoms of VM can be quite disabling and impair the ability to read, drive, walk, and even stand.
What is the cause of vestibular migraine?
The vestibular and migraine networks are very complex. Many scenarios can be proposed. The problem could be that the hyperexcitable migraine brain becomes hypersensitive to motion. Inflammation, including CGRP release, could occur in the vestibular system. Vestibular symptoms could be part of an aura, a wave of electrical activity on the cortex. Research is ongoing.
What treatments can be used for vestibular migraine attacks?
Treatments used for typical migraine attacks (e.g., NSAIDs, triptans) are often used. Since VM can come with severe nausea, antiemetics are often part of the combination. Dizziness can be helped by antihistamine drugs (similar to sea/car sickness medications), although they may cause somnolence.
What medications can decrease the frequency of vestibular migraine attacks?
Migraine preventives are usually tried, with some success. Studies suggest that venlafaxine (Effexor), topiramate (Topamax), and calcium channel blockers (like flunarizine/Sibelium) may be more effective for VM. There are anecdotal reports about Botox improving vestibular symptoms, but more research is needed. Currently, there is no data on CGRP monoclonal antibodies (MABs) and vestibular migraine.
Should I try vestibular physiotherapy?
Vestibular physiotherapy uses exercises to reinforce vestibular reflexes when the ear organs have been injured. The problem with the migraine brain is that it does not manage these reflexes normally, making vestibular physiotherapy challenging and requiring more effort to be effective.
That being said, if there is a diagnosis of benign paroxysmal positional vertigo (BPPV), physiotherapy can be extremely helpful. Additionally, dizziness, vertigo, and migraines are strongly associated with anxiety, which exacerbates these symptoms in a vicious cycle. Therefore, relaxation techniques, meditation, and anxiety management can significantly improve the quality of life for people with VM.
References
- Lempert T, von Brevern M. Vestibular Migraine. Neurol Clin. 2019;37(4):695-706.
Post #106



