Paroxysmal Hemicrania (PH) and Hemicrania Continua (HC) are rare but impactful headache conditions characterized by unilateral pain and distinct autonomic symptoms. Varying in intensity, frequency, and response to treatments, understanding these conditions is crucial for effective management. This article explores their unique features, diagnostic considerations, and long-term treatment approaches, highlighting the necessity of specialized care for optimal outcomes.
My physician has told me that I might have Paroxysmal Hemicrania (PH) or Hemicrania Continua (HC). I have never heard about those before.
PH and HC are very rare. Even headache specialists do not see them very often. They are in the family of trigemino-autonomic cephalalgias, like cluster headache.
Key Characteristics of Paroxysmal Hemicrania and Hemicrania Continua
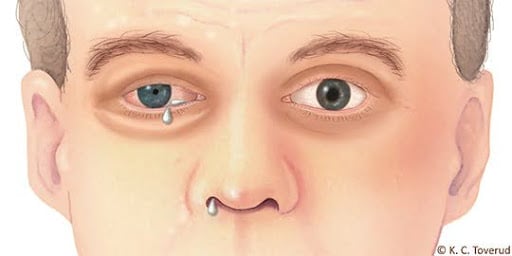
The pain is on one side of the head only: we call these side-locked headaches, or strictly unilateral headaches. There are other symptoms, on the side of the pain: droopy eyelid, teary eye, runny nose, small pupil. We call those “autonomic” as they are mediated by autonomic reflexes.
To read more, see the International Classification Website
Key Differences Between These Headache Conditions
What type of workup should I have if I present those symptoms?
Any patient who presents with these symptoms should see a neurologist. The usual workup will include an MRI. The MRI is expected to be normal. In very rare cases, a benign tumor of the pituitary gland can be linked with TACs. A blood workup could be considered by your physician. It is quite surprising to see such clear symptoms with normal imaging, but remember that migraine and cluster headache are common neurological diseases in which the MRI is also normal.
What is indomethacin and why does it help with these headaches?
Indomethacin is an anti-inflammatory. It has particular effects, including the decrease in the brain pressure and the constriction of blood vessels. At present time science cannot explain why it is so effective to treat certain headaches like paroxysmal hemicrania and hemicrania continua and be relatively ineffective for others like cluster headache and SUNCT.
How should I try the indomethacin?
Your physician will give you the exact instructions, as protocols might vary from one doctor to the other. Usually the dose will start lower (50 mg twice a day) and be increased (up to 200 or even 300 mg per day). Indomethacin is known to cause gastro-intestinal side effects like heartburn and diarrhea. If these side effects are tolerable, it’s best to keep going and at least see if there is a clear improvement that would confirm the diagnosis.
The most important thing to do for a good indomethacin trial is to keep a headache diary and keep count of the daily attacks at baseline and during the treatment. If the effect is 90%, the diary might not be needed, but as the dose increases, a more subtle effect can be observed with the diary.
What will happen to me in the long term if I have a diagnosis of PH or HC?
These headaches can last over decades but may also stop and go into remission. If indomethacin is tolerated, then it will become a long-term treatment, at the lowest dose possible. Sometimes the drug can be stopped for a while (drug holiday). If nerve blocks are helpful, they can be used to spare indomethacin.
If you do develop complications of indomethacin (gastric irritation or ulcers, high blood pressure), you may have to stop it and discuss other options with your physician.
References
- Burish MJ, Rozen TD. Trigeminal Autonomic Cephalalgias. Neurol Clin. 2019;37(4):847-69.
Post #405