Are you new to understanding migraine? This article covers the top ten essential facts about migraine for beginners, shedding light on this complex neurological condition. Despite misconceptions, migraine is a genuine and prevalent disease affecting millions globally. Learn about its diverse symptoms, genetic predisposition, and the need for personalized treatment. Discover how migraine impacts daily life and the support available to those affected. Dive into the world of migraines, debunk myths, and discover the support and community available for those affected by this condition.
- Interconnected Pain Networks
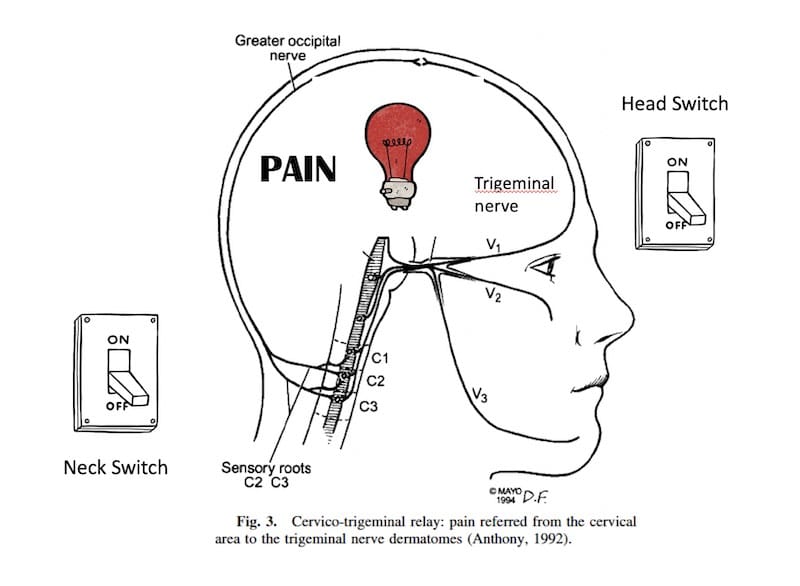
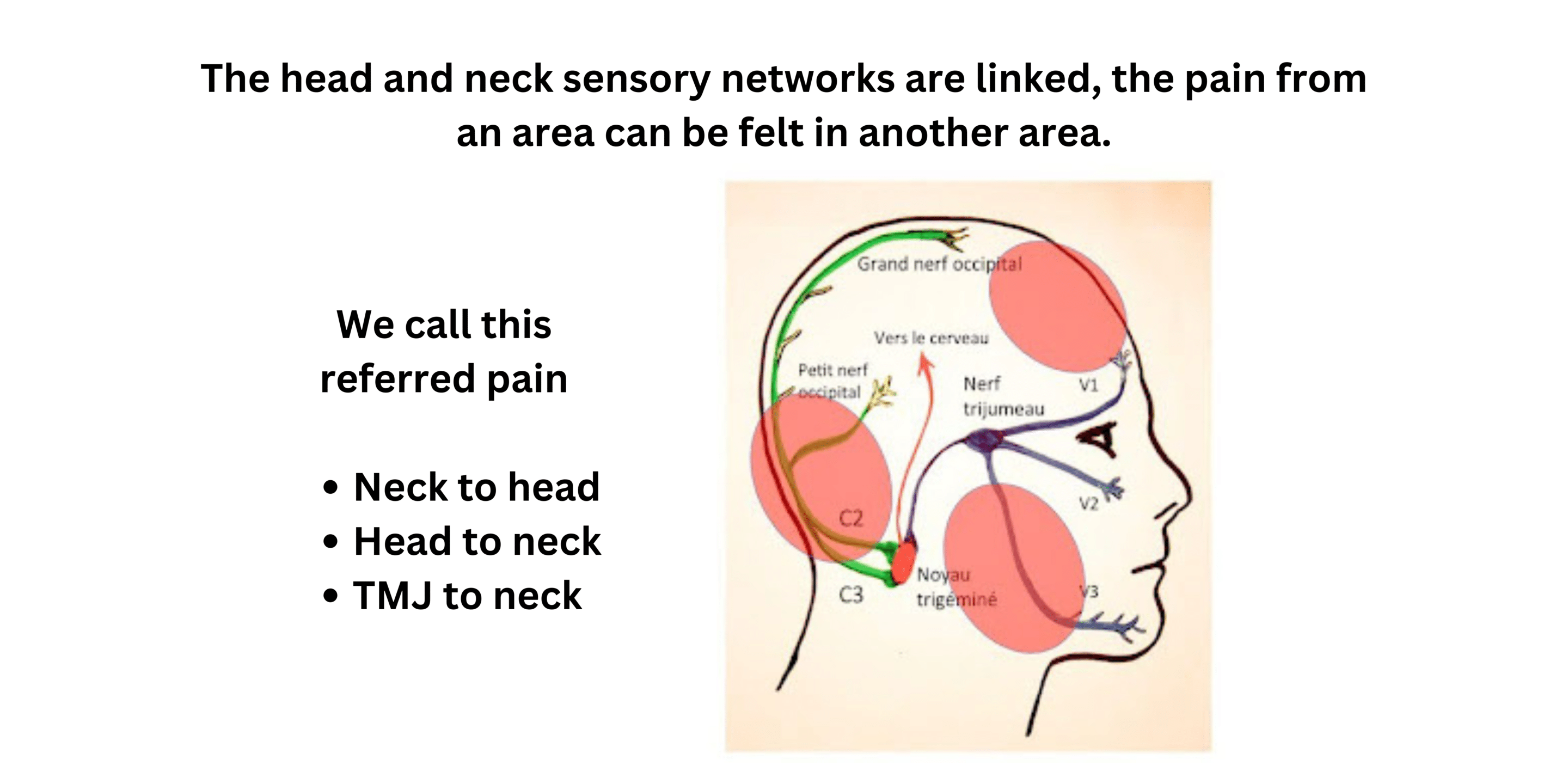
The head and neck pain networks are intricately linked, with signals from the face, head, sinuses, teeth, and jaw carried by the trigeminal nerve, and signals from the neck and upper shoulder carried by the cervical nerves. Both networks converge in the trigeminal nucleus, explaining why head and neck pain often occur together. A neck problem can cause a headache, and vice versa.
- Common Neck Pain in People with Migraine
Around 60% of migraine patients report neck pain during a migraine, even if they have no underlying neck issues. This symptom has been noted since antiquity and is as prevalent as nausea during migraine attacks.
- Limited Usefulness of Imaging Tests
Imaging tests like MRIs often show common age-related changes in neck joints, such as dry disks and arthrosis, which are not necessarily linked to pain. These findings can lead to unnecessary anxiety and further testing, with limited predictive value for treatment responses.
- Complex Neck Structures
The neck is a complex structure with many potential pain sources, including joints, tendons, ligaments, and muscles. Despite this, imaging and clinical examinations often do not provide clear answers, even when conducted by experts.
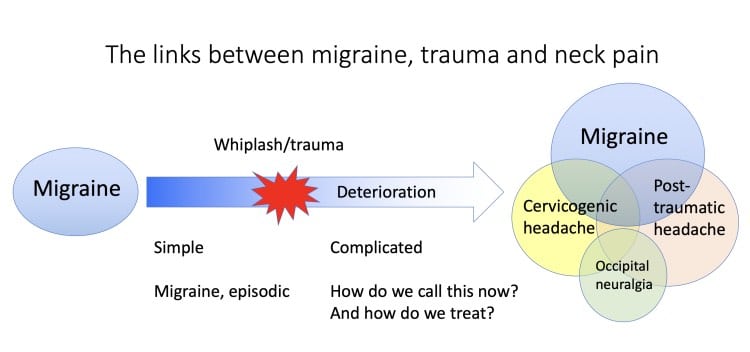
- Cervicogenic Headache and Trauma
Cervicogenic headaches, often resulting from trauma such as concussion or whiplash, are a mixed category in need of clearer definitions. Awareness of this can help patients understand the confusion they might encounter in clinical settings.
- Related Pain Networks
The pain networks of the neck, ear, and jaw are closely related. Problems in one area can cause pain in another, such as a neck issue causing jaw pain or a tooth problem leading to ear pain. Understanding these connections can clarify symptoms.
- Medications and Their Limitations
Medications can help manage chronic neck pain and headache but are rarely sufficient on their own. Options include tricyclics, muscle relaxants, gabapentinoids, NSAIDs, and opioids, though these can lead to habituation, side effects, and dependence.
- The Role of Injections
Injections for neck pain may offer relief, but their effects can often be attributed to a placebo response. Treatments like Botox can help with chronic migraine and associated neck pain but should be administered cautiously to avoid muscle weakening. For more information, visit our Injections and Blocks for Headache: Practical Details post.
- Strengthening Muscles
Strengthening neck and shoulder muscles through regular exercise is crucial for long-term pain management. Passive techniques like TENS machines and massage are less effective. Seeking help from a physiotherapist and committing to a consistent exercise routine over several months is essential for seeing benefits. For more information, visit our Physiotherapy Exercises for Migraine post.
- Long-Term Vision for Pain Management
Neck and back pain are common and should be approached with a long-term strategy. Our sedentary lifestyles and longer lifespans contribute to joint problems. Effective management includes realistic expectations, regular exercise, and stretches, supported by a comprehensive, global approach.
You have only one spine, take good care of it!
References
- Calhoun AH et al. The prevalence of neck pain in migraine. Headache. 2010; 50(8):1273-7.
- Bogduk N, Govind J. Cervicogenic headache: An assessment of the evidence on clinical diagnosis, invasive tests, and treatment. Lancet Neurol. 2009;8(10):959-68.
Post #411



