Dive into the complex neurological roots of migraine. This article explores the genetic, electrical, and chemical components underlying migraine, illuminating their complex interactions within the brain. From the invisible yet tangible nature of migraine on imaging scans to the role of advanced scientific tools like genetics and functional MRI, discover the intricate mechanisms driving this neurological disorder.
Invisible yet tangible
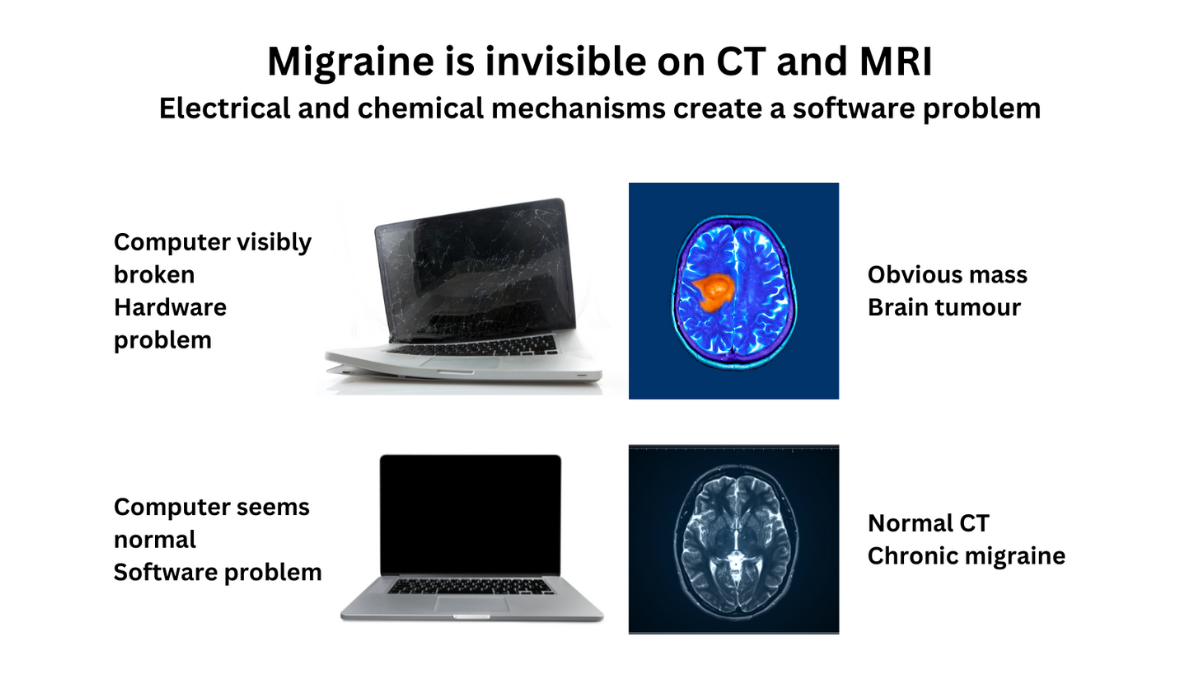
Migraine is not an imaginary problem. It is a complex neurological disease with genetic, electrical, and chemical components. It’s not just “in your head”—migraine involves intricate brain mechanisms. Unlike other brain disorders, migraine isn’t visible on CT scans or MRIs because it involves electrical and chemical signals between neurons, much like software issues in a computer. However, scientific tools like genetics and functional MRI (fMRI) help us understand these mechanisms.
What is the cause of migraine?
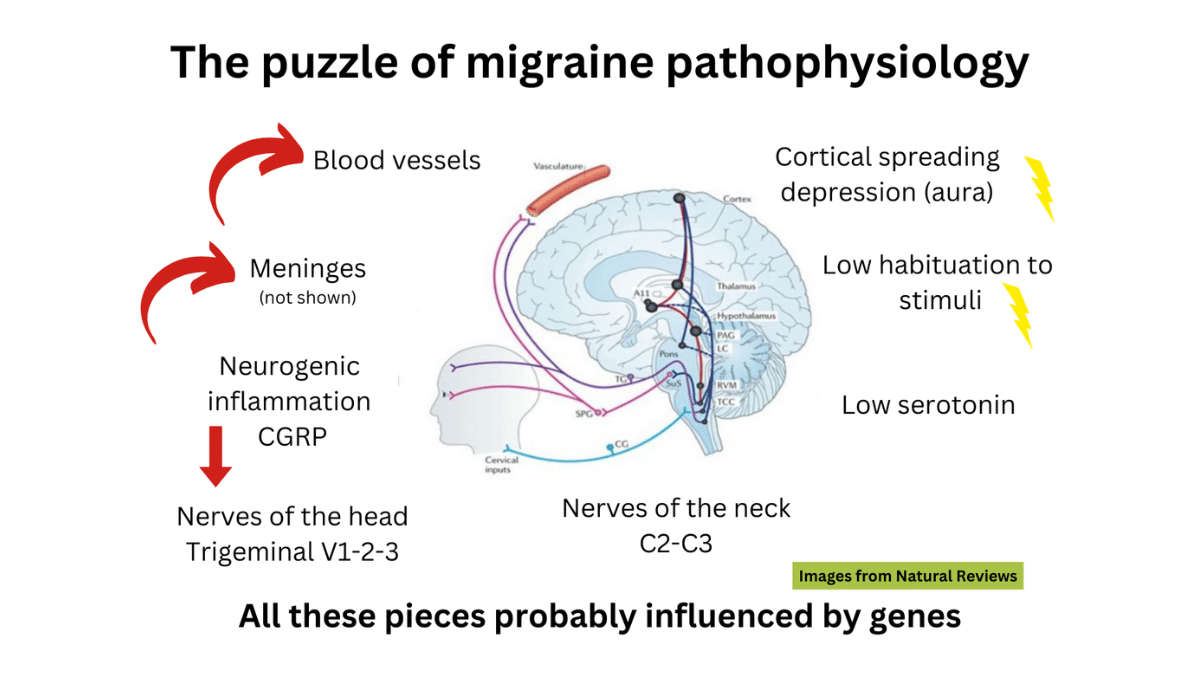
Migraine is a neurological disease, and it has many different mechanisms. We cannot just say “X is the cause of migraine.” We have to look at it like a puzzle with different pieces.
How is migraine studied?
The brain works with electrical and chemical messages between neurons. These mechanisms are not visible to the naked eye or on CT (computed tomography) scans and MRIs (magnetic resonance imaging). You could think of the electrical and chemical messages as software in a computer. Migraine is like a software problem, where the computer still looks fine, but the programs are not functioning because the messages are not being sent properly.
Luckily, there are different scientific tools to study migraine.
The pieces of the migraine puzzle
Like a puzzle, there are many sections to how migraine works depending on which tool is used to study it. These tools include genetics, fMRI (functional magnetic resonance imaging), substances that trigger or prevent migraine, and immunology.
Multiple genes have been associated with migraine
We do not yet understand the role of all those genes. Most are involved in the function of neurons and blood vessels. We think that migraine has different ways of presenting in different people because so many genes are involved. Some forms of migraine are linked with one precise gene, for example hemiplegic migraine. For more information, visit our Hemiplegic Migraine post.
The migraine brain does not adapt to repeated stimuli
If you flash a light in the eyes of a person without migraine repeatedly, their brain will eventually decrease its response. For people with migraine, the brain keeps reacting again and again. Observations of this lack of adjustment have been made with light and sound. This may lead to people with migraine spending more energy being aware of our environment. In theory, an overload of stimulation could then lead to an attack.
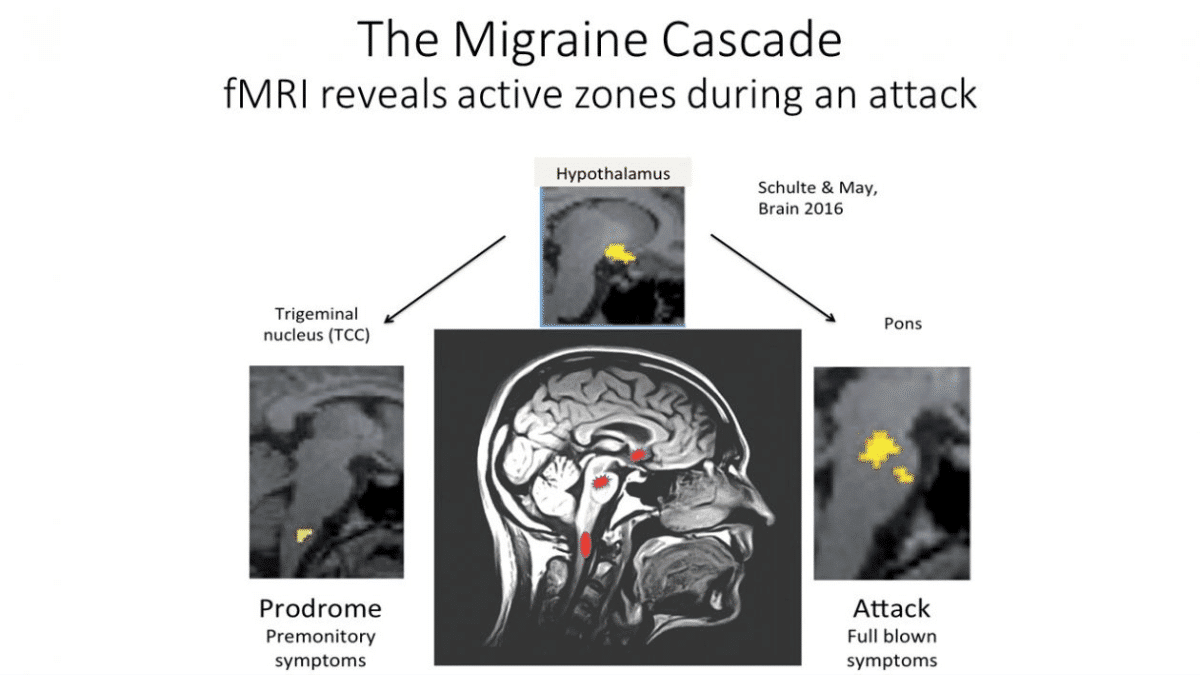
During the migraine attack, different brain zones light up (the migraine cascade)
In studies using fMRI, we can see the brain zones active during a migraine, including the hypothalamus (manage hormones and cycles), trigeminal nucleus (pain signals), and the pons (modulate serotonin and pain).
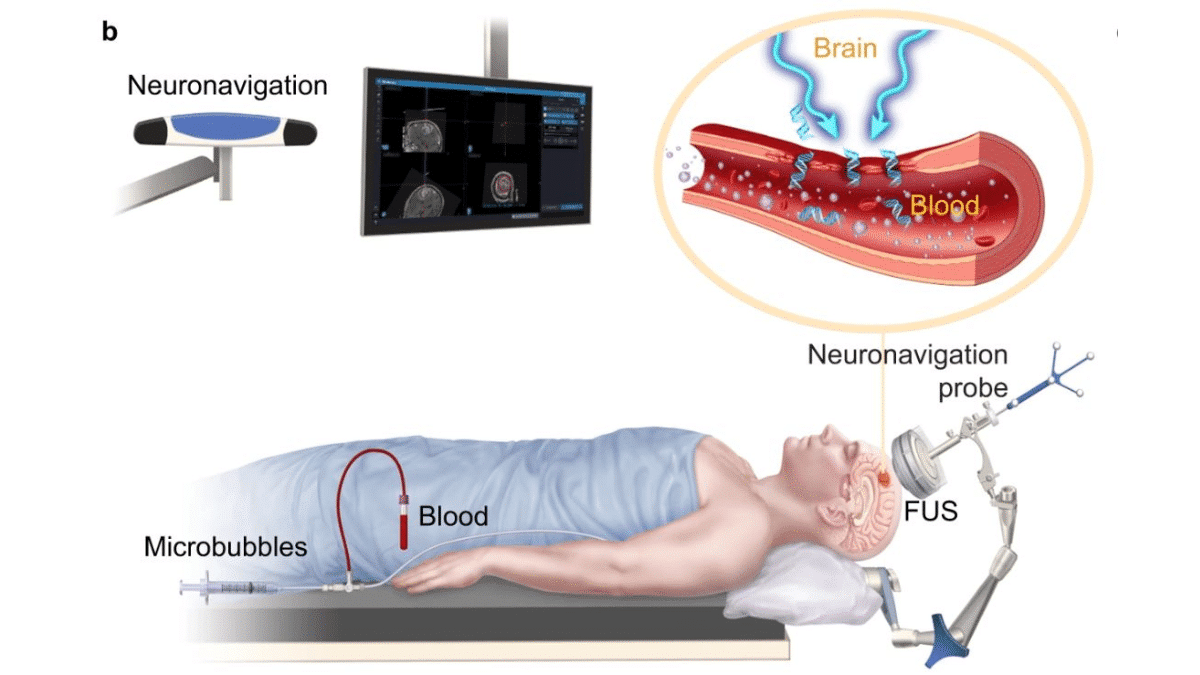
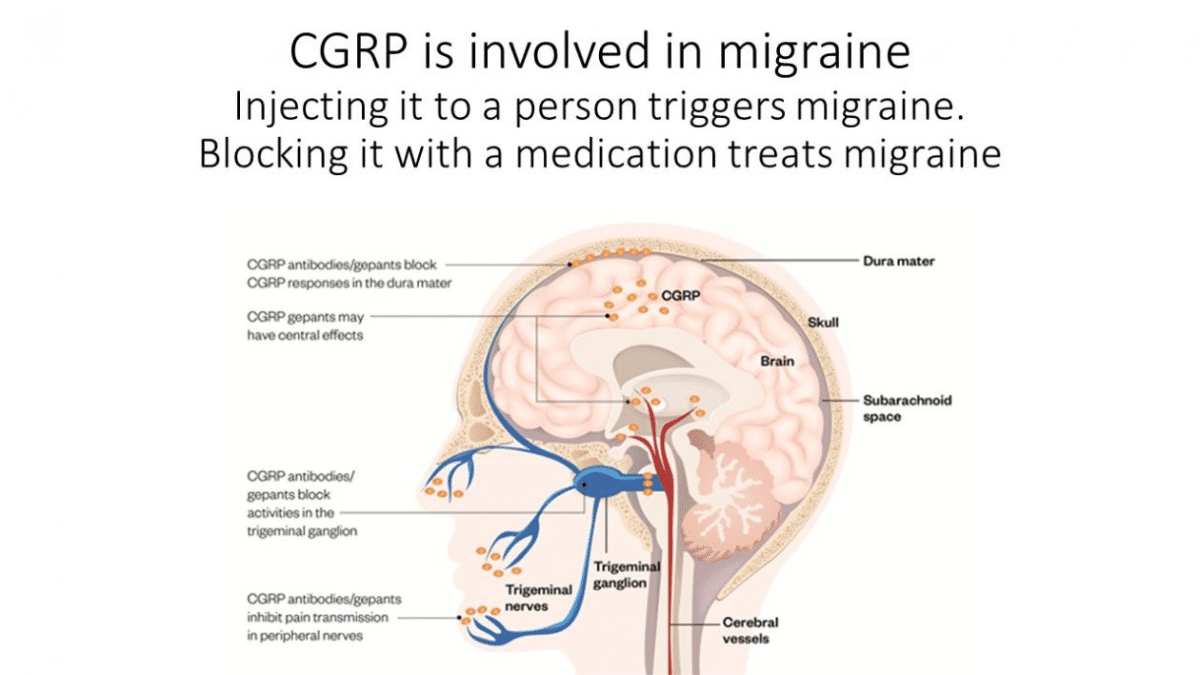
Chemicals and proteins can trigger migraine attacks when injected into a person’s blood
For centuries, it was believed migraine was caused by the dilation of blood vessels. Treatments were aimed at constricting blood vessels to ease the migraine pain. Now we know the truth is more complicated. The dilation of the vessels may trigger an attack but may also be the consequence of the attack. To study migraine, researchers inject people with substances such as CGRP (calcitonin gene related peptide) to trigger an attack.
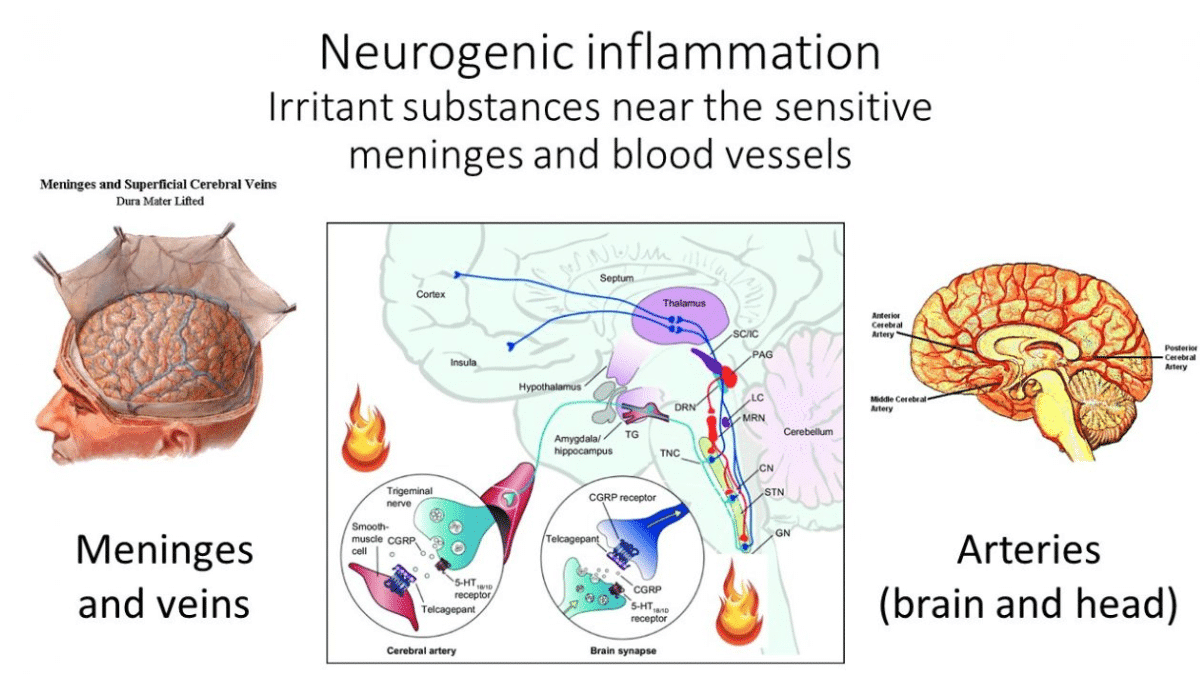
Migraine pain comes from irritated membranes and blood vessels
The migraine attack leads to a release of inflammatory substances in the brain near the arteries and the membrane (the meninges) that surrounds your brain. That’s where the pain comes from, but our body does not have a map to tell us where our arteries and meninges are. So instead, the pain is felt in the eyes, temples, sinuses, and neck.
What is CGRP and what role does it play in migraine?
CGRP (calcitonin gene related peptide) is one of the inflammatory substances that is involved in the migraine attack. CGRP dilates blood vessels and causes pain.
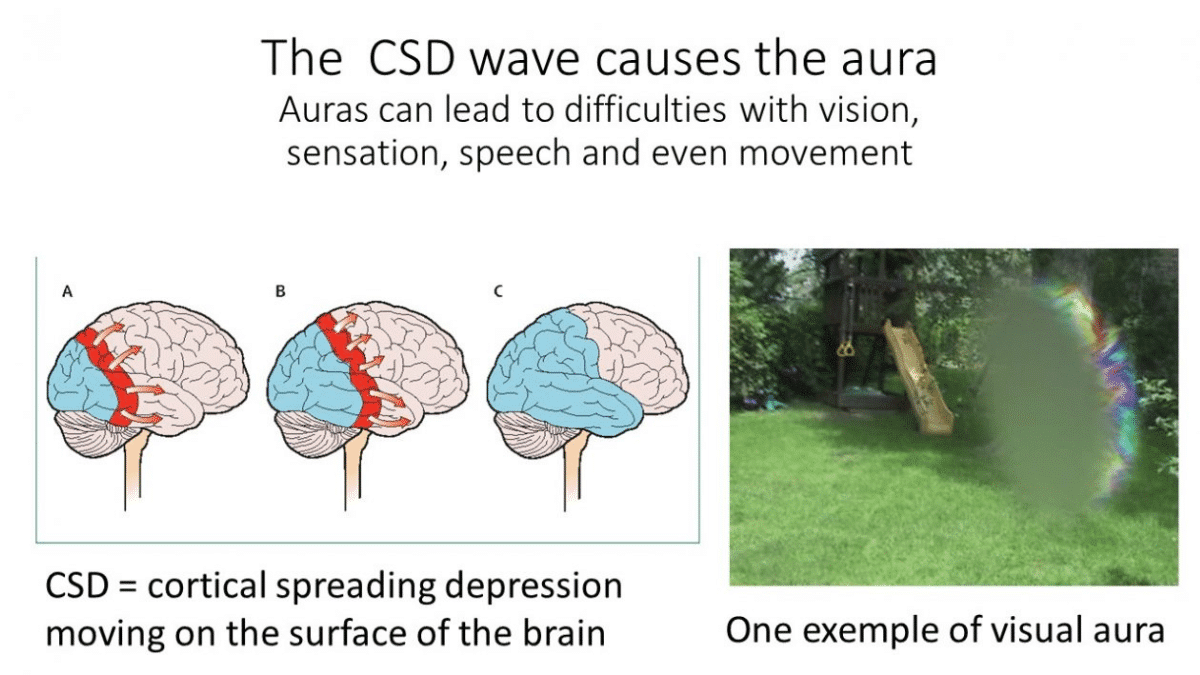
What is the cause of the aura?
Migraine aura is caused by cortical spreading depression (CSD), an electrical wave that alters neuron and blood vessel activity. Symptoms vary depending on where the wave travels in the brain. Most auras are visual, but some involve speech difficulties and strange sensations on one side of the body. For more information, visit our Migraine With Aura post.
Serotonin is low in the migraine brain between attacks, and spikes during the attack
Serotonin is a hormone that plays different roles in the body. It constricts the blood vessels and it is also involved in many brain activities. Serotonin plays a role in mood, and low serotonin is associated with depression. Serotonin is made in the pons, one of the brain zones active during a migraine attack. Triptans treat migraine attacks by acting on serotonin receptors to relieve pain. For more information, visit our History of Triptans.
Conclusion
The science of migraine has progressed significantly, uncovering the intricate workings of our brains. Continued research promises even greater insights and more effective treatments.
References
- Charles AC, Baca SM. Cortical spreading depression and migraine. Nat Rev Neurol. 2013;9(11):637-44.
- Goadsby PJ, Holland PR, Martins-Oliveira M, Hoffmann J, Schankin C, Akerman S. Pathophysiology of Migraine: A Disorder of Sensory Processing. Physiol Rev. 2017;97(2):553-622.
- Sutherland HG, Albury CL, Griffiths LR. Advances in genetics of migraine. J Headache Pain. 2019;20(1):72.
- Edvinsson L. The Trigeminovascular Pathway: Role of CGRP and CGRP Receptors in Migraine. Headache. 2017;57 Suppl 2:47-55.
- Deen M, Christensen CE, Hougaard A, Hansen HD, Knudsen GM, Ashina M. Serotonergic mechanisms in the migraine brain – a systematic review. Cephalalgia. 2017;37(3):251-64.
- Ashina M, Hansen JM, BO AD, Olesen J. Human models of migraine – short-term pain for long-term gain. Nat Rev Neurol. 2017;13(12):713-24.
- Schulte LH, May A. The migraine generator revisited: continuous scanning of the migraine cycle over 30 days and three spontaneous attacks. Brain. 2016;139(Pt 7):1987-93.
- de Tommaso M, Ambrosini A, Brighina F, Coppola G, Perrotta A, Pierelli F, et al. Altered processing of sensory stimuli in patients with migraine. Nat Rev Neurol. 2014;10(3):144-55.
- Sakai Y, Dobson C, Diksic M, Aube M, Hamel E. Sumatriptan normalizes the migraine attack-related increase in brain serotonin synthesis. Neurology. 2008;70(6):431-9.
Post #007