Migraine Causes and Triggers
On this page, we answer these questions:
What do we know about the cause of migraine?
What is the cause of auras?
How do we study migraine?
What is the difference between the cause of migraine and a migraine trigger?
Migraine is not an imaginary problem.
Migraine is a neurological disease with genetic components and electrical and neurochemical mechanisms.
Because of the many different mechanisms and genetic components involved, we cannot just say “X is the cause of migraine”. We have to look at it like a puzzle with different pieces. Although it is complex, research is active and unveiling the ways our brain works.
Read below to learn what we know so far, and how researchers are working to discover more!
We are still discovering new things about what causes migraine.
Here is what we know so far.
Multiple genes have been associated with migraine.
Multiple genes have been associated with migraine. We do not yet understand the role of all those genes. Most of them are involved in the function of neurons and the function of blood vessels. We think that migraine has different ways of presenting in different people because so many genes are involved. Some forms of migraines are linked with one precise gene (for example, hemiplegic migraines).
The migraine brain does not get used to repeated stimulations.
If you flash a light in the eyes of a person without migraine repeatedly, their brain will eventually decrease its response. For people with migraine, the brain keeps reacting again and again. Observations of this lack of adjustment have been made with light and sound. This may lead to people with migraine spending more energy being aware of our environment. In theory, an overload of stimulation could then lead to an attack.

During a migraine attack, different brain zones light up (the migraine cascade).
In studies using fMRI, we can actually see the brain zones active during a migraine. These zones include the hypothalamus, the trigeminal nucleus and the pons (see diagram). The hypothalamus is the manager of all our hormones and cycles, including sleep. The trigeminal nucleus integrates pain signals from the head and neck, and the pons contain zones that modulate pain and serotonin.
Different chemicals and proteins can trigger migraine attacks when injected into a person’s blood.
For centuries, migraine was thought to be caused by the dilation of blood vessels. Treatments aimed to constrict blood vessels to ease migraine pain. Now, we know the truth is more complicated. The dilation of the vessels may trigger an attack but may also be the consequence of the attack. In order to study migraine attacks, researchers inject people with inflammatory substances such as CGRP (calcitonin gene-related peptide, which dilates blood vessels) to trigger an attack.
The migraine pain comes from irritated membranes and blood vessels.
The migraine attack leads to a release of inflammatory substances inside the brain. This release takes place near the arteries and the membrane (the meninges) that surrounds your brain. That’s where the pain comes from, but our body does not have a map to tell us where our arteries and meninges are. So instead, the pain is felt in the eyes, temples, sinuses and neck.
What, then, is the cause of an aura?
The aura is caused by an electrical wave in the brain called “cortical spreading depression” or CSD. The cortical spreading depression leads to changes in the activity of the neurons and the blood vessels. Depending on where this wave goes on the brain surface, the symptoms vary. Most auras are visual, but some involve speech difficulties and strange sensations on one side of the body.

Migraine is not visible on CT scans and MRIs, so how can we study it?
The brain works through electrical and chemical messages between neurons, which are not visible to the naked eye or on CT (computed tomography) scans and MRIs (magnetic resonance imaging). You could think of the electrical and chemical messages as software in a computer. A brain tumour is like a hardware problem, which is much easier to see. Migraine is like a software problem, where the computer still looks fine, but the programs are not functioning because the messages are not being sent properly.
Luckily, there are different scientific tools to study migraine. These include genetics, fMRI (functional magnetic resonance imaging), substances that trigger or prevent migraine, and immunology.
Electricity –
We use electrophysiological recordings and electroencephalogram (EEG) to study electric activity in the cells
Chemistry –
We use blood levels and biomarkers to study proteins, neurotransmitters and Ion channels.
Genetic –
We use gene testing and genome-wide scans to measure DNA and chromosomes.
Active brain zones –
We use functional MRI (fMRI) and PET scans to study blood flow in real-time in certain zones.
Macroscopic –
We use CT scans and MRIs to study brain matter, meninges, arteries, and so on.
What is the difference between the cause of migraine and a migraine trigger?
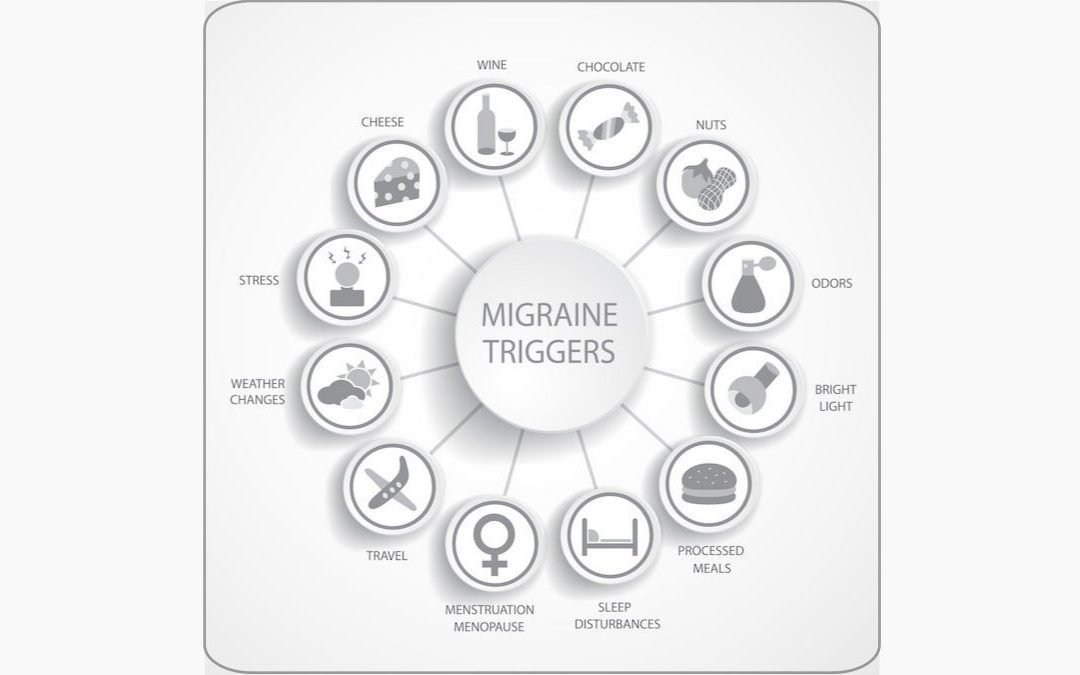
Migraine is a neurological disorder that predisposes people to migraine attacks. As noted above, the cause is genetic, and these genetic changes result in changes in brain chemistry that lead to the migraine tendency. Triggers, on the other hand, are things that tend to bring on migraine attacks in people who are predisposed to have them. Triggers, which can range from weather changes, hormonal changes, stress, or chemicals in certain foods seem to upset the chemical balance in the brain of those with migraine and make it more likely that they will have a migraine attack. Sometimes, one trigger is not enough to trigger an attack, and two happening at the same time can add up and do so.
Even though you cannot change your genes and therefore cannot eliminate your tendency to have migraine attacks, triggers can very much influence how frequent your attacks will be. That is why it is important to develop a lifestyle that reduces your chances of having a migraine attack. For example, learning how to manage stress better can help as stress is one of the things that many with migraine say is one of their most important attack triggers.
Read more on Migraine Triggers & Lifestyle Adaptations

How Food and Nutrition Can Impact Migraine
Curious about how food can impact your migraine? Food is often the first line of defense against migraine, but it’s important to remember there's no one-size-fits-all approach to diet. This...
The Ping Pong Theory: Is Migraine a Cause or a Consequence?
Understanding whether migraine is a cause or a consequence of various factors is crucial for effective management. This article on the Ping Pong Theory delves into the complex interplay between the...
Migraine Triggers: Avoid or Cope?
Migraine attacks can be triggered by various factors. While it’s impossible to avoid all triggers, identifying your specific ones through a migraine diary can be helpful. Understanding the...
How to stay active and avoid triggering migraine attacks
Research shows that regular movement and exercise benefits everyone and can improve migraine symptoms. However, many people with migraine find it challenging to stay active. This resource offers...

Sleep and migraine: Improve your sleep without medication
Sleep and migraine often feed off each other—poor sleep can trigger a migraine, and a migraine attack can disrupt your rest. Enhancing your sleep quality is a crucial step toward managing your...
Does Brain health improve Migraine Health?
Welcome to Migraine Canada's "Ask Your Pharmacist" webinar series, where we explore critical topics beyond medications and conditions. In this episode, Dr. Crystal Culler, founder of the Virtual...
Communication & Advocacy Strategies when living with migraine
Discover essential insights on managing migraine through effective communication and support strategies in this insightful webinar from Migraine Canada. Whether you're a migraine patient navigating...

Sleep and Migraine – Webinar
Welcome to Migraine Canada’s "Ask Your Pharmacist" webinar series! In this episode, we are thrilled to have Rachel Luther, a dedicated and passionate pharmacist from Center Wellington Remedies RX,...
The Science of Migraine: “It’s All in Your Brain” – Part 1
Welcome to Migraine Canada, your source of support and information for navigating life with migraine. In this community, we explore insights, tips, and strategies to empower you in managing...
Get More Information
How is migraine
diagnosed?
As the research on migraine grows, our ability to diagnose it improves – but there are still many challenges. Get the latest information on how migraine is diagnosed in Canada, and what that means for you.
How can I support migraine research?
Continued research into the causes of migraine can help to improve the lives of millions of Canadians. Join Migraine Canada to advocate for progress and make a difference.
What about other types of headaches?
Migraine Canada advocates for research and understanding of all types of headaches, including but not limited to those caused by migraine. Learn more from our resources on other headache causes.
References
Charles AC, Baca SM. Cortical spreading depression and migraine. Nat Rev Neurol. 2013;9(11):637-44.
Goadsby PJ, Holland PR, Martins-Oliveira M, Hoffmann J, Schankin C, Akerman S. Pathophysiology of Migraine: A Disorder of Sensory Processing. Physiol Rev. 2017;97(2):553-622.
Sutherland HG, Albury CL, Griffiths LR. Advances in genetics of migraine. J Headache Pain. 2019;20(1):72.
Edvinsson L. The Trigeminovascular Pathway: Role of CGRP and CGRP Receptors in Migraine. Headache. 2017;57 Suppl 2:47-55.
Deen M, Christensen CE, Hougaard A, Hansen HD, Knudsen GM, Ashina M. Serotonergic mechanisms in the migraine brain – a systematic review. Cephalalgia. 2017;37(3):251-64.
Ashina M, Hansen JM, BO AD, Olesen J. Human models of migraine – short-term pain for long-term gain. Nat Rev Neurol. 2017;13(12):713-24.
Schulte LH, May A. The migraine generator revisited: continuous scanning of the migraine cycle over 30 days and three spontaneous attacks. Brain. 2016;139(Pt 7):1987-93.
de Tommaso M, Ambrosini A, Brighina F, Coppola G, Perrotta A, Pierelli F, et al. Altered processing of sensory stimuli in patients with migraine. Nat Rev Neurol. 2014;10(3):144-55.
Sakai Y, Dobson C, Diksic M, Aube M, Hamel E. Sumatriptan normalizes the migraine attack-related increase in brain serotonin synthesis. Neurology. 2008;70(6):431-9.
Post#7
