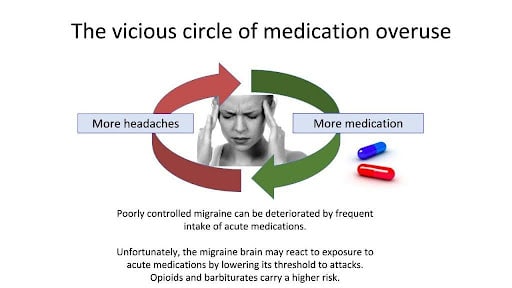
For those grappling with frequent migraine attacks, relying on acute medications seems like a logical solution. However, this can lead to a lesser-known complication called medication overuse headache (MOH). MOH occurs when the medications used to alleviate headaches are taken too frequently, inadvertently exacerbating the problem they were intended to solve. Explore the causes, risk factors, and implications of MOH, and learn how recognizing and managing this condition can lead to significant improvements in your migraine management strategy.
How do we know that MOH exists?
Headache experts began seeing MOH when analgesics became easily accessible. They observed that some people who had developed chronic headaches could significantly improve after stopping the regular intake of their medications. Many studies have shown this.
Is MOH a common problem? Am I the only one?
MOH is thought to affect 1 to 2% of the general population, so yes, it is common, and no, you’re not the only one. 60 million people worldwide suffer from this. It may surprise you, but MOH is one of the top 20 causes of disability worldwide, according to the World Health Organization.
How much medication could lead to MOH?
According to the International Headache Classification:
- Ten days per month for triptans, opioids, and any mix of medication.
- Fifteen days per month if you use acetaminophen or NSAIDs ONLY.
Many experts set the limit at treating 2-3 days per week to stay on the safe side, but many people with clear MOH use acute treatments more than 20 days per month or almost daily.
Are these numbers absolute limits?
No. These numbers are based on statistics in studies showing an association between frequent intake of acute medications and chronic headaches. In some people, this frequency of intake may lead to chronification. In others, it might be higher or lower frequencies. Some people with migraine might even use daily acute medications without developing MOH.
So, it’s possible to overuse without having a medication overuse headache?
Yes. The term “medication overuse” describes a frequent intake exceeding the official limits. The term “medication overuse headache” is used if there is evidence or a strong impression that the overuse contributes to chronic headaches. This being said, overuse is a serious issue and should be addressed. You should never assume that overuse is not a problem unless a withdrawal has been completed.
What’s the cause of MOH?
The migraine brain has a particular chemical software. Genes are involved. We know that if it is exposed to medications acting on pain networks, the pain networks change, and pain increases. People without migraine do not seem to react this way to acute medications. For example, in a group of patients taking daily Tylenol for arthritis, only the ones with a history of migraine developed MOH. Unfortunately, the people who need the medications are the ones developing problems by using them.
Am I more at risk for MOH?
There are risk factors for MOH. Interestingly, the risk factors are very similar to the ones linked to chronic migraine in general.
-
Not modifiable: Female gender, other chronic pain, age < 50 years old, high intensity of headaches, and a low educational level.
-
Modifiable: Obesity, lack of exercise, smoking, use of tranquilizers and opioids, anxiety, and depression.
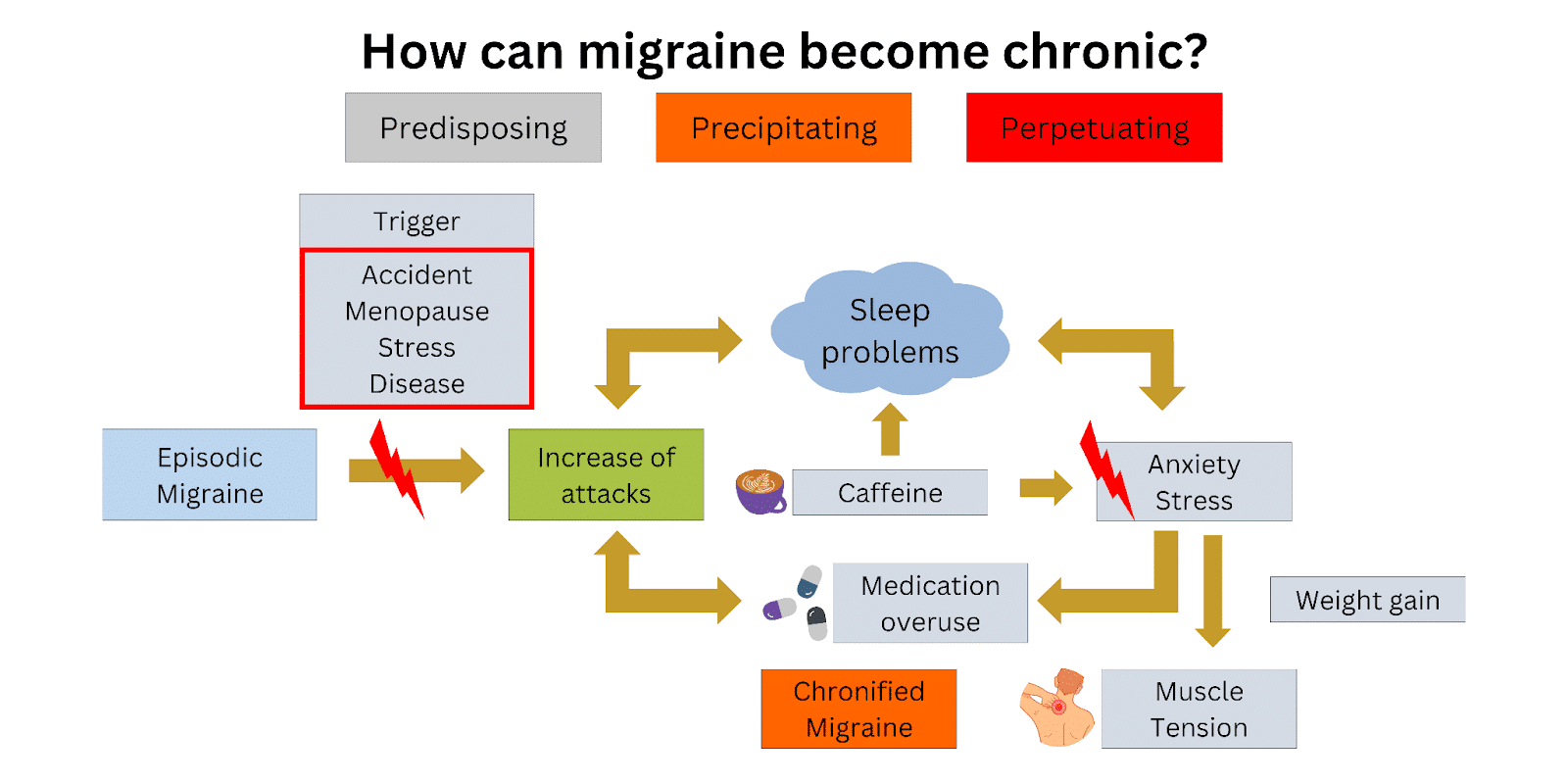
I am using my meds because I have frequent headaches…what’s the cause, and what’s the consequence?
Excellent question. It is a chicken-and-egg situation. Having frequent migraine attacks is also a major risk factor in chronification. It can be difficult to tell which came first, the frequent medication use or the increase in headaches. There can be multiple causes for chronification. The only way to know if medication use is a cause for you is to stop and see if your headaches improve.
How can I know if I have MOH?
First, look at your current situation with a migraine diary. Record your attack frequency and any intake of acute medication. If you use analgesics or opioids for other pain, include them. Then, ask yourself these questions:
- Am I using acute medications more than 10-15 days per month?
- Am I using more acute medications than I did in the past?
- Has my migraine become more frequent?
- Are my medications less effective?
- Do I have a lingering daily headache, possibly worse in the morning?
I think I may have MOH. What do I do now?
You’ve taken the first step by recognizing the issue, and that’s great! There is hope for improvement. To start, please read our detailed guide on how to plan a medication withdrawal.
Remember, you can do this!
References
- Diener HC, Holle D, Solbach K, Gaul C. Medication-overuse headache: risk factors, pathophysiology and management. Nat Rev Neurol. 2016;12(10):575-83.
- Fischer MA, Jan A. Medication-overuse Headache (MOH). StatPearls. Treasure Island (FL): StatPearls Publishing
- StatPearls Publishing LLC.; 2019.
- Schwedt TJ, Chong CD. Medication Overuse Headache: Pathophysiological Insights from Structural and Functional Brain MRI Research. Headache. 2017;57(7):1173-8.
- Scher AI, Rizzoli PB, Loder EW. Medication overuse headache: An entrenched idea in need of scrutiny. Neurology. 2017;89(12):1296-304.
Post#804