Chronic migraine can be a challenging and debilitating condition, affecting daily life and well-being. Proper diagnosis, understanding symptoms, and recognizing risk factors are key to effective management. This guide explores the complexities of chronic migraine, offering valuable insights into diagnosis criteria, potential risk factors, and strategies to help manage and improve this challenging condition.
How does the physician diagnose chronic migraine?
If you have a history of occasional migraine and the attacks have become more frequent over months or years, so that you now have a headache for more than 15 days a month, then a diagnosis of chronic migraine is possible. Another cause must be ruled out by appropriate investigation, but chronic migraine remains the most common cause of chronic headache.
Simply put, you must have:
- A history of migraine with or without aura
- 15 days of headache per month
- 8 days are migraine (the other may look like tension type)
- This situation must be there for at least 3 months
- No other cause for the headaches
What if I have good months and bad months, and my frequency is sometimes 8 and sometimes 17?
Remember that migraine frequency fluctuates, and many patients may have a very bad month in the “chronic” category, then go back down to episodic. We call this the roller coaster of migraine.
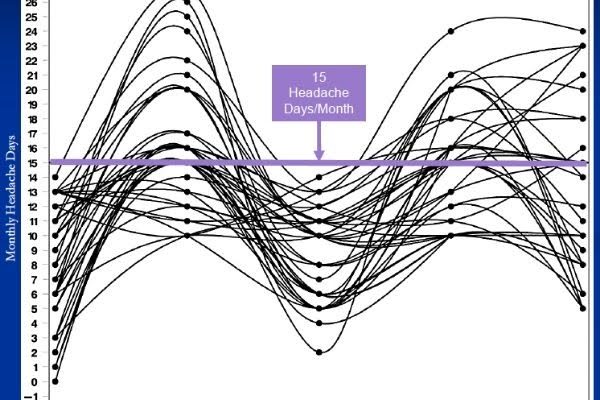
For this reason, some researchers now believe that putting people with migraine into boxes does not represent the true continuum of migraine. It may be important for research to create categories, but real life is more complicated.
I heard that migraine is a chronic disease… even in the episodic form.
That is correct. “Chronic” may have two meanings. It can mean “for a long time,” and even episodic migraine may last for decades, affecting the person from childhood to older age. But “chronic migraine” in the International Classification of Headache Disorders (ICHD) refers to the frequency of the attacks. This can be somewhat confusing.
I seem to have a mix of migraine and tension headache… is it chronic migraine?
People with chronic migraine often report headaches of different intensities: low-intensity headaches that can be there almost daily, some moderate attacks, and some severe attacks. According to the ICHD, 8 days per month have to be clearly migrainous to diagnose chronic migraine.
If you’d like to read more about this topic and learn about the 0-1-2-3 approach to tracking headaches, see this post.
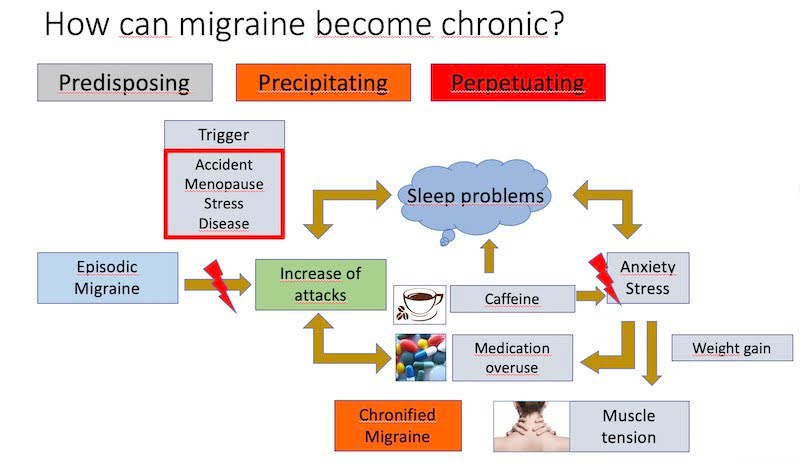
What are the risk factors for developing chronic migraine?
- Being born female
- Diabetes, arthritis, other chronic pain
- High frequency of attacks in recent months
- History of trauma to the head or neck
- Sleep problems
- Obesity
- Depression
- Regular intake of caffeine
- Overuse of acute medication
Another way to picture the vicious circles of chronic migraine is illustrated below. This is why working on lifestyle can be very beneficial.
If I overuse acute medications, do I have only medication-overuse headaches?
No. You have chronic migraine AND medication overuse. Overuse is added to chronic migraine and must be managed, as it is not always the key factor for the deterioration of migraine. Appropriate treatment is essential.
Can chronic migraine be reversed?
Good news: chronic migraine can transform back into episodic migraine. Approximately 25% of people with chronic migraine will return to an episodic state after 2 years. If chronification is caused by a treatable factor, migraine can improve.
Is chronic migraine a cause of disability?
Migraine (even in its chronic form) is not listed as a cause of disability in Canada. Individuals may need to base their claims on associated conditions like depression or anxiety.
Is chronic migraine caused by depression?
People with chronic migraine are more likely to experience depression and anxiety, with anxiety having a stronger association. It’s important to seek treatment if you suffer from these conditions.
Is chronic migraine caused by neck problems?
Chronic migraine is more common in individuals who have suffered head trauma or whiplash injury. The complex nervous system can link chronic pain in one area of the body to developing pain in other areas.
What should healthcare providers know about treating chronic migraine?
For treating migraine, healthcare providers can refer to the work of Drs. Robinson, Hird and Sandoe, and Rizoli (see references below). Their work details how to diagnose and treat migraine, as well as considerations for medication overuse headache.
In conclusion, chronic migraine is a severe disabling form of migraine that should be treated with a global approach.
References
- Rizzoli P. Medication-Overuse Headache. Continuum (Minneap Minn). 2024 Apr 1;30(2):379-390.
- Hird MA, Sandoe CH. Medication Overuse Headache: An Updated Review and Clinical Recommendations on Management. Curr Neurol Neurosci Rep. 2023 Jul;23(7):389-398.
- Robinson, G. Identifying and Treating Chronic Migraine. Canadian Journal of Diagnosis. 2015 Oct: 43-46.
- Buse, D.C. Migraine Progression: A Systematic Review. Headache. 2019;59(3):306-38.
- Becker WJ. The Diagnosis and Management of Chronic Migraine in Primary Care. Headache. 2017;57(9):1471-81.
- Adams AM, et al. The impact of chronic migraine: The Chronic Migraine Epidemiology and Outcomes (CaMEO) Study methods and baseline results. Cephalalgia. 2014.
- Diener HC et al. Chronic migraine–classification, characteristics and treatment. Nat Rev Neurol. 2011;8(3):162-71
Post #102