What is Idiopathic Intracranial Hypertension (IIH)?
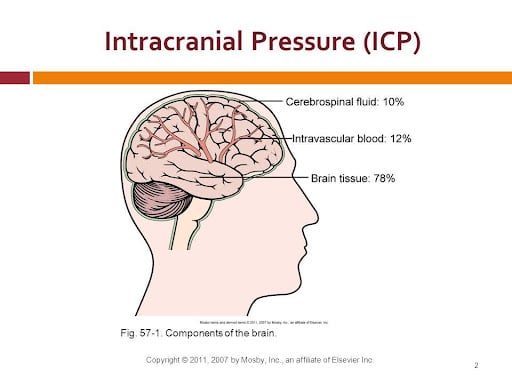
Idiopathic Intracranial Hypertension (IIH), also known as pseudotumor cerebri, is a condition where the pressure inside the skull increases without an obvious cause. Normally, intracranial pressure should remain stable, similar to how a car tire maintains pressure. If the pressure is too low, it can cause issues such as intracranial hypotension syndromes. Conversely, if the pressure is too high, it can lead to significant damage.
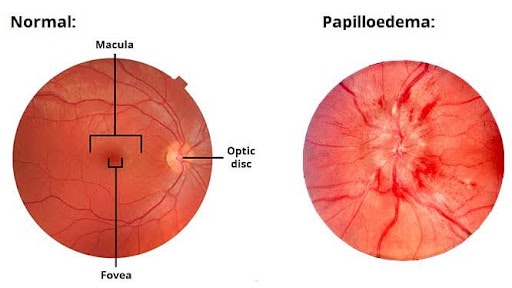
IIH disrupts the mechanisms that regulate this pressure, resulting in headaches and swelling of the optic nerves, which can threaten vision.
Common Symptoms of IIH
The primary symptom of IIH is a headache, experienced by 90% of patients. This headache is usually diffuse, moderate, and sometimes throbbing, often worsening when lying down due to increased pressure. Additional symptoms include:
- Nausea and vomiting
- Visual disturbances: This includes seeing black when bending over, seeing stars, and losing peripheral vision, due to optic nerve swelling.
- Double vision (diplopia): Caused by pressure on the nerves controlling eye movement.
- Tinnitus: Ringing in the ears, which can be pulsatile and exacerbated by lying down or bending over.
Causes of IIH
The exact cause of IIH is unknown, but it is hypothesized that the brain accumulates too much fluid, leading to increased pressure.
Diagnosis of IIH
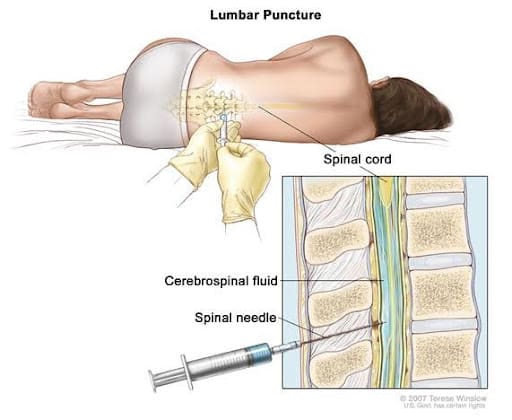
If symptoms suggest IIH, a neuro-ophthalmologist should evaluate the optic nerves and visual fields for swelling (papilledema) and vision loss. An MRI of the brain and a lumbar puncture to measure intracranial pressure are essential for diagnosis. If optic nerves appear normal and pressure isn’t elevated, other chronic headache causes, like chronic migraine, should be considered.
Other Causes of High Intracranial Pressure
Several conditions can raise intracranial pressure, including:
- Masses in the brain: Such as tumours or abscesses.
- Venous thrombosis: Blockages in veins, which require imaging (CT or MRI) to diagnose.
- Coagulation disorders: Linked with conditions like lupus.
- Certain medications: For example, Accutane and some antibiotics.
IIH and Migraine Connection
Around 40% of people with IIH have a history of migraine, higher than the general population’s 15%. IIH is more common in women of reproductive age, who are also more prone to migraines. Physicians may recommend treatments like topiramate and Botox for headache control in these patients.
The Role of Weight Loss in Managing IIH
Obesity is strongly linked with IIH. Losing weight, even as little as 10% of body weight, can significantly improve symptoms and protect vision. Weight loss is challenging, but crucial for managing IIH. Learn more about weight loss strategies by visiting our post Weight Loss: Tips for People with Migraine.
Medications for IIH
- Acetazolamide: A diuretic that can improve vision but may not be as effective for headaches. Side effects include nausea, tingling in extremities, and fatigue.
- Methazolamide: Similar to acetazolamide but potentially better tolerated.
- Topiramate: Used for epilepsy and migraines, it may help with headaches and promote weight loss but has side effects like memory and focus difficulties.
- Avoid weight-gain inducing drugs: Such as amitriptyline (Elavil).
Surgical Options: Shunting
In severe cases where vision is at risk, surgical shunting may be considered. This involves placing a tube to drain fluid from the brain ventricles to the abdomen (ventriculo-peritoneal shunt) or from the spine to the abdomen (lumbo-peritoneal shunt). These procedures carry high risks and should only be performed by experts.
Preventing Vision Loss in IIH
Regular eye exams by an ophthalmologist or optometrist are essential. If symptoms worsen, immediate vision testing is necessary to monitor the optic disk and visual fields.
For more information on Idiopathic Intracranial Hypertension, visit the National Eye Institute.
References
- Ahmad SR, Moss HE. Update on the Diagnosis and Treatment of Idiopathic Intracranial Hypertension. Semin Neurol. 2019;39(6):682-91.
- Friedman DI. Contemporary management of the pseudotumor cerebri syndrome. Expert Rev Neurother. 2019;19(9):881-93.
- Ganesh A. Idiopathic intracranial hypertension: need to rule out cerebral venous sinus thrombosis. Cmaj. 2019;191(40).
- Thurtell MJ. Idiopathic Intracranial Hypertension. Continuum (Minneap Minn). 2019;25(5):1289-309.
Post #403



