Headache and neck pain: is it possible that nerve compression is to blame?
Headache and neck pain: is it possible that nerve compression is to blame?
A team of researchers investigates the possibility of a surgical approach
Patient story: my neck is killing me
«For the last few years, my neck has been killing me. I had migraines since the age of 15 but they were occasional. Slowly, things deteriorated. True enough, I am always sitting at work and I stopped exercise a few years ago. My posture is not good. The chiro helps me for a while, but then it comes back. Of course I can’t do anything with my arms in the air for too long. Sometimes, it’s this pressure in the neck, going to the shoulders. Sometimes, the baseball bat, then a full blown migraine. Is this my life? Can’t I just be fixed somehow?»
Why would a neck problem cause a headache?
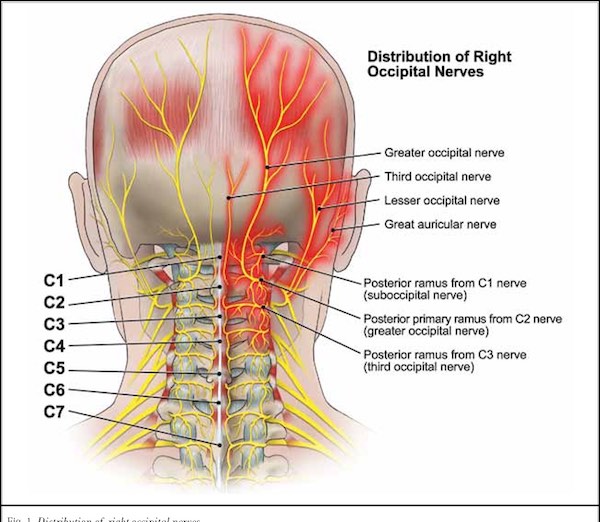
The nerves of the neck and the head all connect in the same place in the brain. Two zones that are especially linked are the forehead/temples (V1) and the occiput and higher neck (C2-C3). From the human anatomy perspective, the head and the neck are the same pain zone. The link can go both sides: a neck problem can cause headache, and a headache can induce neck pain.
I heard that migraine was a disease of the brain…where is the neck in this puzzle?
Migraine is a disease of the brain. We know that the migraine brain has chemical and electrical characteristics, and that many genes play a role in this special «software». This is the «central» theory of migraine, where the key culprits are the brain networks.
This being said, the brain is always reacting to the environment, and pain signals are able to turn on the migraine cascade. The neck is a site of pain directly plugged into the brainstem zones for headaches. It’s not a surprise then that neck pain could trigger migraine attacks.
What prompted the researchers to study this topic of neck and headache?
Patient stories and symptom description. Both Dr Blake and Burstein were aware that
• Many patients with headache also complain of neck pain.
• These people were not much improved by medications acting on the brain.
• Interventions targeting the neck were sometimes useful, including manipulations, blocks and even surgeries.
Of course, one has to be careful before jumping to conclusions about the effectiveness of surgeries, as the placebo effect associated with them is very high. Nevertheless, this idea that targeting the neck could help some patients could not be completely discarded.
What could cause a compression of the occipital nerves?
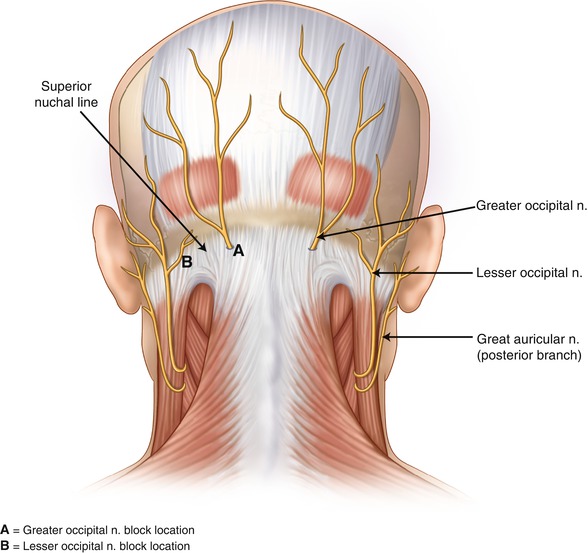
The occipital nerves (greater and lesser) go through different layers of muscle before making it to the skin of the occiput. Multiple compression sites have been shown by anatomical and surgical studies. Sadly, we do not yet have imaging techniques to see compressions. Even the MRI is not able to demonstrate it.
What did the researchers do to prove their theory?
Dr Burstein, Dr Blake and their teams embarked on a true scientific journey.
Studies were done on animals, and then humans, to understand the anatomy of the neck nerve fibers better. They demonstrated that some nerve fibers for the neck cross the skull to go inside and connect to the meninges. They observed signs of compression of these nerves during surgery. They also showed that there are signs of inflammation in the nerves of people with chronic migraine. We can compare this vision to the problem of sciatica, where a compressed nerve root leads to pain in the leg and in the lumbar spine.
The idea is that inflammation of the nerves from the neck could lead to inflammation inside the back of the head, and that this could cause chronic headaches. In a person with migraine, this inflammation could trigger more attacks and chronification. This would be an example of the «peripheral theory of migraine».
Should we consider surgery (decompression of the occipital nerves) to treat migraines?
The researchers published seven patient stories after surgery. Some patients improved significantly, others did not. The challenge now is to predict who could really do better with a surgery and which surgery exactly. As we do not have very good imaging techniques to see the cervical nerves anatomy, this is difficult. Symptoms are also variable and people may express theirs in many different ways. The physical examination of the neck is complex, as when the pain is there, it’s difficult to tell where it’s from just by pushing on the occiput. The question of placebo must be addressed, as physicians should not expose people to surgeries that are not truly effective.
What’s the conclusion? Should I look for a surgery?
The issue of neck pain linked with headaches and migraine is an important one. Too many patients are disabled by these symptoms. Any doctor seeing headache patients and willing to listen knows about this. But science is based on observation of facts, not only symptoms and hypotheses. It is too early to say that decompressive surgeries should be use in practice, but the research must continue. This therapeutic option could become an official one after sufficient testing.
References:
Emerging evidence of occipital nerve compression in unremitting head and neck pain
Blake, Burstein et al, The Journal of Headache and Pain (2019) 20:76
Tracking patients with chronic occipital headache after occipital nerve decompression surgery: A case series.
Blake, Burstein et al., Cephalalgia. 2019 Apr;39(4)
Categories
THE MIGRAINE TREE
- BRANCHES
- ACUTE TREATMENTS
- DEVICES AND NEUROMULATIOIN
- PREVENTIVE TREATMENTS
- PROCEDURES AND INJECTIONS
- SELF-CARE AND LIFESTYLE
- SOCIAL LIFE
- TRUNK
- ROOTS
OTHER CATEGORIES