Early life expressions of migraine
Which early life conditions may be related to migraine?
There are a few conditions named «episodic syndromes that may be associated with migraine». These were previously called «childhood migraine equivalents» because they are associated with migraine in adulthood and share common points with migraine. In the International Classification of Headache Disorders (https://ichd-3.org/), the following syndromes are listed:
These conditions affect 1-3% of children. They occur between the ages of 2 to 8 years old, commonly starting around 3-4 years old. They tend to resolve with adolescence but may persist in some people during adulthood.
Other conditions commonly seen during childhood which may be related to migraine include infant colic (See this post) and motion sickness. These conditions may also occur without any link to migraine.
These disorders have the following common key features:
- On and off (periodic) timing
- The child feels normal between attacks
- Attacks can be triggered by things that may trigger migraine a swell: exhaustion, stress, lack of sleep, fasting, certain foods etc.
- There is a family history of migraine (65-100% of children have an affected parent)
- Children with these conditions are more likely to develop migraine as they grow up compared to patients who do not have these conditions: 25% of children with migraine equivalents (on a mean) will develop migraine compared to 15% in the general population.
- Paroxysmal torticollis and vertigo may be associated with cyclical vomiting and/or abdominal migraine, so these syndromes seem to overlap.
How are these conditions diagnosed?
Diagnosis is based on symptoms and by ruling out other possible causes that could be dangerous or may require a specific treatment. Different specialists might be involved.
Awareness of these syndromes leads to the correct diagnosis, avoids unnecessary tests and improves treatment. Invasive testing in children with strong family history of migraine may not be needed. It is not rare to see a child being investigated for a long time in gastro-enterology or going repeatedly to the emergency department when the diagnosis could be made by a pediatric neurologist. Collaboration is key in the management of these disorders.
What treatments are available?
The first priority is establishing the diagnosis and reassuring patients and their families that the conditions are not dangerous. Treatment includes eliminating triggers, lifestyle and behavior strategies as well as acute treatment of the specific attack. Long term prevention may require medicines. Please read more detailed chapters for each syndrome (Post#602, Post#603, Post#604, Post#606)
Will it improve? Will my child have migraines in the future?
Most of these syndromes improve and may go away over time. Unfortunately, some kids with abdominal migraine and cyclic vomiting syndrome continue in adulthood.
Even if these syndromes are considered precursors of migraine, not all children will develop migraine in the future.
| Have a family history of migraine | Will develop migraine ** | |
| Cyclical vomiting | 28-82% | 20-35% |
| Abdominal migraine | 35-90% | 70% |
| Paroxysmal torticollis | 40-80% | Up to 41% |
| Paroxysmal vertigo | 40-100% | 15-70% |
** Different studies show different results, so there is no absolute prediction for evolution to migraine.
REFERENCES:
- Gelfand A. Episodic syndromes of childhood associated with migraine. Current Opinion Neurology.2018;31:281-285.
- Lagman-Bartolome AM, Lay C. Pediatric Migraine Variants: A review of epidemiology, diagnosis, treatment and outcome. Current Neurology and Neuroscience.2015;12:1-14.
Post#601
Categories
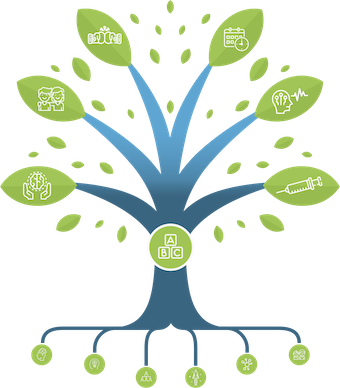
THE MIGRAINE TREE
- BRANCHES
- ACUTE TREATMENTS
- DEVICES AND NEUROMULATIOIN
- PREVENTIVE TREATMENTS
- PROCEDURES AND INJECTIONS
- SELF-CARE AND LIFESTYLE
- SOCIAL LIFE
- TRUNK
- ROOTS
OTHER CATEGORIES